Latest News Update 20.1
April 13, 2022
Dear Patients
This is our latest news update following on from our last one in December. Previous updates issued throughout the course of the pandemic can be found here.
It has been quite some time since the last update - we've been so busy over the Christmas and New Year period whilst also having to cope with severe short-staffing through sickness and stress and also having had to manage the covid vaccination booster campaign at the beginning of the year.
It's a big issue this time, so please take your time in reading it at your leisure.
FACE COVERINGS
FACE COVERINGS STILL NEEDED IN HEALTHCARE SETTINGS
With the easing of restrictions of Plan B on January 27, 2022, the legal requirement to wear masks was removed.
However, we still require anyone over the age of 11 years to wear a face covering when entering the building. This is because, under health and safety legislation, we have an overriding legal duty to protect all patients and staff within our building.
Risk assessments have shown that masks are still required, therefore we kindly ask that all our patients abide with the request to continue to wear face coverings in a healthcare setting.
Please note that visors are not suitable and do not provide any protection to either the wearer or to those around them.
The following is an extract from official and current government guidance:
Please also see the following official BMA poster below left:
FACE COVERINGS PROTECT OUR STAFF AND KEEP OUR SERVICE RUNNING
We know that there are a tiny proportion of patients who do not wish to comply with such requirements, but we hope that you can all understand that face coverings are not really for you, they are there to help to protect others around you, including our staff.
You will all know that the legal requirement to self-isolate has also been removed, however, what you might not know is that frontline healthcare workers who have covid must still continue to self-isolate - this is because healthcare settings are high risk areas that run the risk of an outbreak developing.
Therefore, if you do not wear a face covering, you risk exposing our staff to covid and this then has the potential to severely and adversely affect our ability to provide you with a service. This has been very aptly illustrated in recent weeks, where, not only have we had a doctor already off sick, but the locum doctors booked to replace them have also been off sick with covid.
We therefore ask for your help in keeping everyone safe in the surgery when you attend. If you refuse to wear a face covering and have no valid reason for exemption, we will not refuse to see you if it is deemed clinically appropriate, however, we will kindly ask you to leave the premises whilst we agree with you alternative arrangements for you to be assessed or examined.
This might mean an assessment elsewhere, or by other method, including remotely, or in a specifically equipped clinical room, or even in the car park. This is to ensure the safety and security of our staff and other patients who are in your immediate vicinity.
ABUSE REGARDING FACE COVERINGS WILL NOT BE TOLERATED
We remind all patients that violent or abusive behaviour regarding face coverings, or any other issue for that matter, will not be tolerated whatsoever in accordance with our compliance with NHS Zero Tolerance Policy.
IVY.GS: Face coverings page GOV: When to wear a face covering IVY.GS: Zero tolerance policyINFORMATION FOR NEW PARENTS
Dr Greer introduces a page she has written for new parents
Becoming a new parent can be a rewarding but challenging experience. We realise that there are so many changes that occur in the first few weeks and months of your baby’s life that trying to remember appointments and get the support you need can be difficult.
We have set up a text message alert system to direct all new parents to a page on our website with all the information you may need about what appointments are needed for you and your baby in the first few months of life. There are also links to various resources nationally and locally for help with things such as breastfeeding, contraception and mental health. We also include links to various leaflets devised by Ivy Grove Surgery with helpful information such as how to know when your child is poorly and useful contact numbers that you may need.
We hope that this information is helpful to new parents. If you have used or come across any local baby groups or resources you have found helpful in your parenting journey then please let us know and we would be happy to add them to our page so that other parents may benefit from them.
IVY.GS: New baby page IVY.GS: How can I tell if my child is poorly? leafletCOVID UPDATES
COVID STILL VERY MUCH OUT THERE
Just because covid is no longer in the news, doesn't mean it has disappeared. Just because it is a mild illness in most people doesn't mean that getting it won't make an impact. With nearly 1 in 10 people with covid and with hundreds of deaths every day still and with thousands of people having to take time off from work or school, it is far from over.
CHANGES TO TESTING
More specifically, there is no free testing anymore, either lateral flow (LFD) or PCR.
From April 1, 2022, free universal symptomatic (PCR tests) and asymptomatic testing (LFD tests) will be discontinued for the general public in England.
NHS: Changes to testing for coronavirus in EnglandA small number of people will still be able to get free lateral flow tests on the NHS:
- If you have a health condition which means you're eligible for new COVID-19 treatments - see link below
- If you're going into hospital for surgery or a procedure - your hospital will tell you how to get a test
- If you work in the NHS or in social care - see link below
NHS: Treatments for coronavirus and eligibility GOV: Order coronavirus rapid lateral flow tests
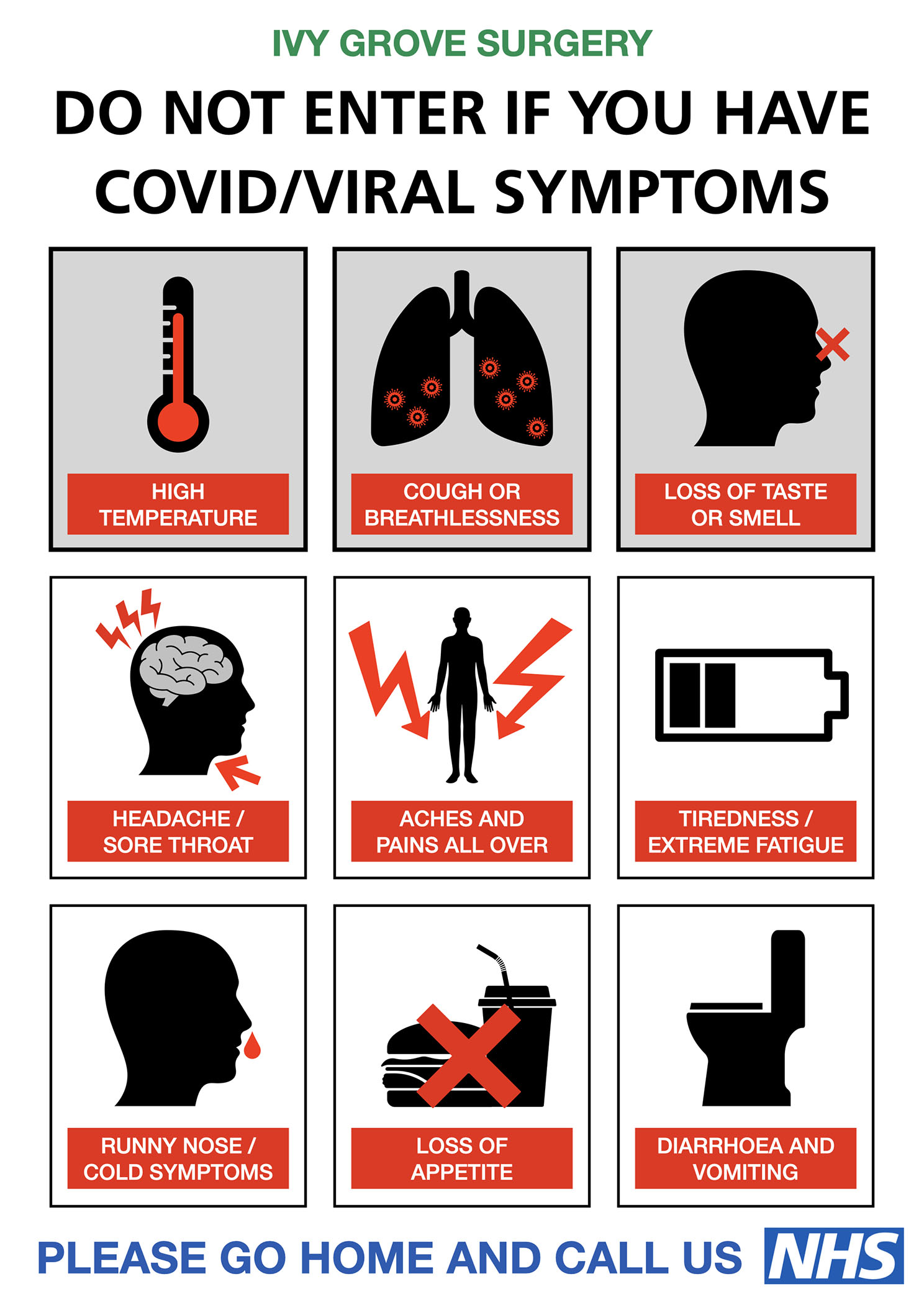
COVID SYMPTOMS LIST EXPANDED
The official list of covid symptoms has now been expanded from the original three of temperature, cough and loss of sense of smell or taste, which we have had for over two years. Whilst some would say this decision is a somewhat backwards step given that free covid testing has come to an end for most people, the full list is however welcome from a medical point of view if it actively encourages people to consider whether the condition they have is covid or not.
- Continuous cough
- High temperature, fever or chills
- Loss of, or change in sense of taste or smell
- Shortness of breath
- Unexplained tiredness, lack of energy
- Muscle aches or pains
- Not wanting to eat or not feeling hungry
- Headache that is unusual or longer lasting than usual
- Sore throat, stuffy or runny nose
- Diarrhoea, feeling sick or being sick
If you have the above symptoms and you have a high temperature or you do not feel well enough to go to work or carry out normal activities, you are advised to try to stay at home and avoid contact with other people. These leads us on to the next topic.
NHS: What to do if you have coronavirusDON'T COME TO SURGERY WITH COVID
We need to remind all patients, if you have active covid, please do not come to surgery, even if you are wearing a face covering. This is so that we can keep other patients and our staff safe, some of whom will be highly clinically vulnerable.
Also, as mentioned before, we simply cannot afford to have staff off self-isolating with covid, as we still need numbers in order to provide a safe and efficient service.
If you have a booked appointment but have since developed covid, or are awaiting the result of a test, or are self-isolating, please do not attend your appointment. Please ring us to cancel, and we will agree with you an alternative method of providing you with the care that you need.
Please check symptoms above, or view the above poster which provides a quick summary of what to look for.
IVY.GS: Covid symptoms poster NHS: Stay at home guidance for covid infectionIF YOU OR YOUR CHILD IS POORLY WITH COVID
If you have covid and you are worried about your symptoms or you are not sure what to do, please use the online service (this is official advice):
NHS: Get medical helpFor a baby or child under 5, call 111 if you're worried (this is official advice):
Ring 111If your child seems very unwell, is getting worse or you think there's something seriously wrong, call 999 (this is official advice):
Ring 999COVID VACCINATION
The following groups remain eligible for covid vaccination:
- 1st and 2nd doses for people aged 12 years old and over
- Boosters for people aged 16 years old and over, plus at-risk children aged 12 to 15 years old
- Spring boosters for people aged 75 years old and over, plus people aged 12 years old and over with a weakened immune system
- Additional primary doses for people with a severely weakened immune system aged 12 years old and over
We are working on getting patients invited to the Church Farm hub so if you are in the above groups you can wait for your invite or if you prefer, you wish to book for your booster using NHS services straight away you can click either button below:
NHS: book booster online Ring 119 to book booster IVY.GS: Covid booster pageCORONAVIRUS ADVICE PAGE
Given the huge changes that are happening to the guidance, and a change in testing, milder cases and a move towards 'Living with Covid', we have taken to decision to decommission our coronavirus advice page. The page has served its usefulness, being visited regularly by you, our patients, but also having reached many thousands of other patients all over the UK, having been linked to by other surgery websites.
But the time has come to start to move away from it. As part of the process, we will continue to link to official sources of gov.uk and nhs.uk information that you can still refer to:
GOV: Living with Covid GOV: Get a PCR test if you have symptoms NHS: How to look after yourself at home GOV: Info for healthcare workersMENTAL HEALTH SUPPORT
We know that it can be very distressing when you are suffering with poor mental health - you may not know what you need to do, or what sort of help is available or whom you need to approach.
At the start of the pandemic, we set up our mental health page to point you in the right direction. We have continued to expand and develop this page as time goes on as it has proved an invaluable resource for all affected patients.
NEW PAGE LAYOUT
We have now completely revamped our mental health support pages to provide easier access to help and resources.
You can access the mental health support page via various methods:
- On a desktop machine, click the link at the top of the page: Mental health support
- On a mobile device, open the menu top right then:
- From the left hand menu, click and choose Mental health support
- From any main page of our website, click the button: GET MENTAL HEALTH SUPPORT
We also know it can be very overwhelming to be presented with such a lot of information, therefore we strongly encourage you to take your time when visiting the page and/or ask a trusted friend or relative to help.
IVY.GS: Mental health support pageNEW SECTIONS - CRISIS AND SELF-HARM
We have also added specific 'In a crisis' and 'Self-harm' sections to our mental health page. These sections provide more information on what you can do to start to get the help that you need when you are really suffering and are at risk.
To access these, click the buttons marked 'In a Crisis' or 'Self-harm'.
IVY.GS: Mental health support pageNEW ADDITION - GRIEF SUPPORT
We have added the following link to the 'Adults/General' section of our mental health page. The Good Grief Trust exists to help all those affected by grief in the UK. The aim of the trust is to help those bereaved from day one, acknowledge their grief and provide reassurance, a virtual hand of friendship and ongoing support.
The trust brings bereavement services together, to ensure that everyone receives the tailored support they need to move forward with their lives.
From their website, you can find local resources, specific information on loss and lots of useful articles and inspirational videos.
The Good Grief TrustNEW ADDITION - RETHINK RESOURCES
Many factors in health and wellbeing are determined by our environment, our social network, our relationships, our work, our financial situation and so on, that cannot be solved by a doctor's prescription. Whilst we will always try and help people medically, we do encourage all patients to try and improve their health and wellbeing with additional support.
To this end, in our 'Adults/General' section, we have added some new resources from ReThink to help support people with activity, peer support, socialising and keeping active. We hope you find these useful.
Ceramics group (Zoom) Drop-in (Belper) Group Interest Central Grow Outside (Ripley) Info Hub (Ripley) Pool and Coffee Meet Wellbeing Singing Group (Ripley) Sport and Swim for Wellbeing (Amber Valley) Tech Buddies Volunteer to be a Tech BuddyWe also encourage patients to read the inspiring story from one of our patients, Scott, below and also find out about our new Health and Wellbeing Coach.
Scott's Running Madness IVY.GS: Health and wellbeing coach pageGENERAL PRACTICE NEWS
The situation in GP land continues to be very precarious.
SERVICE IS UNDER IMMENSE PRESSURE
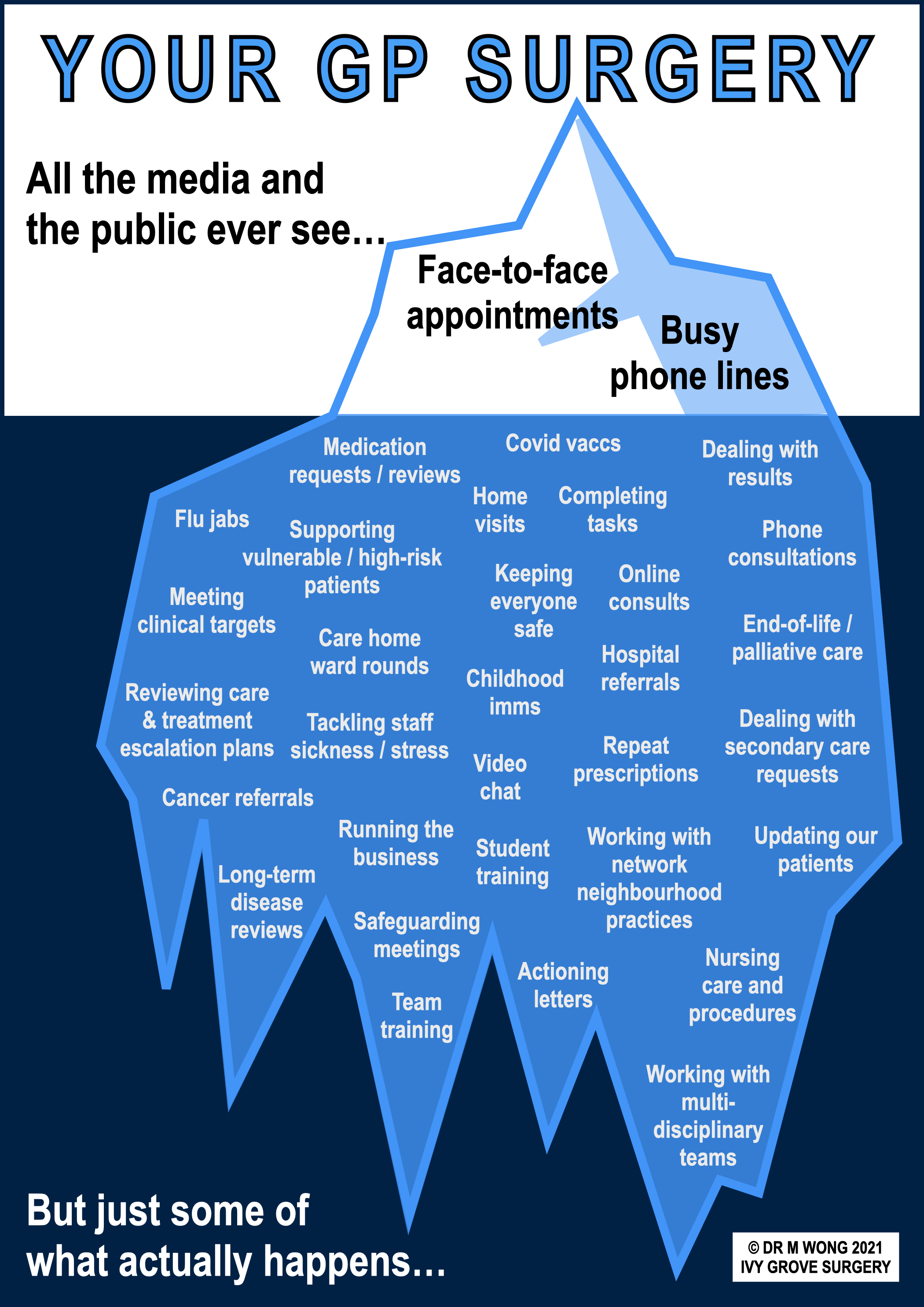
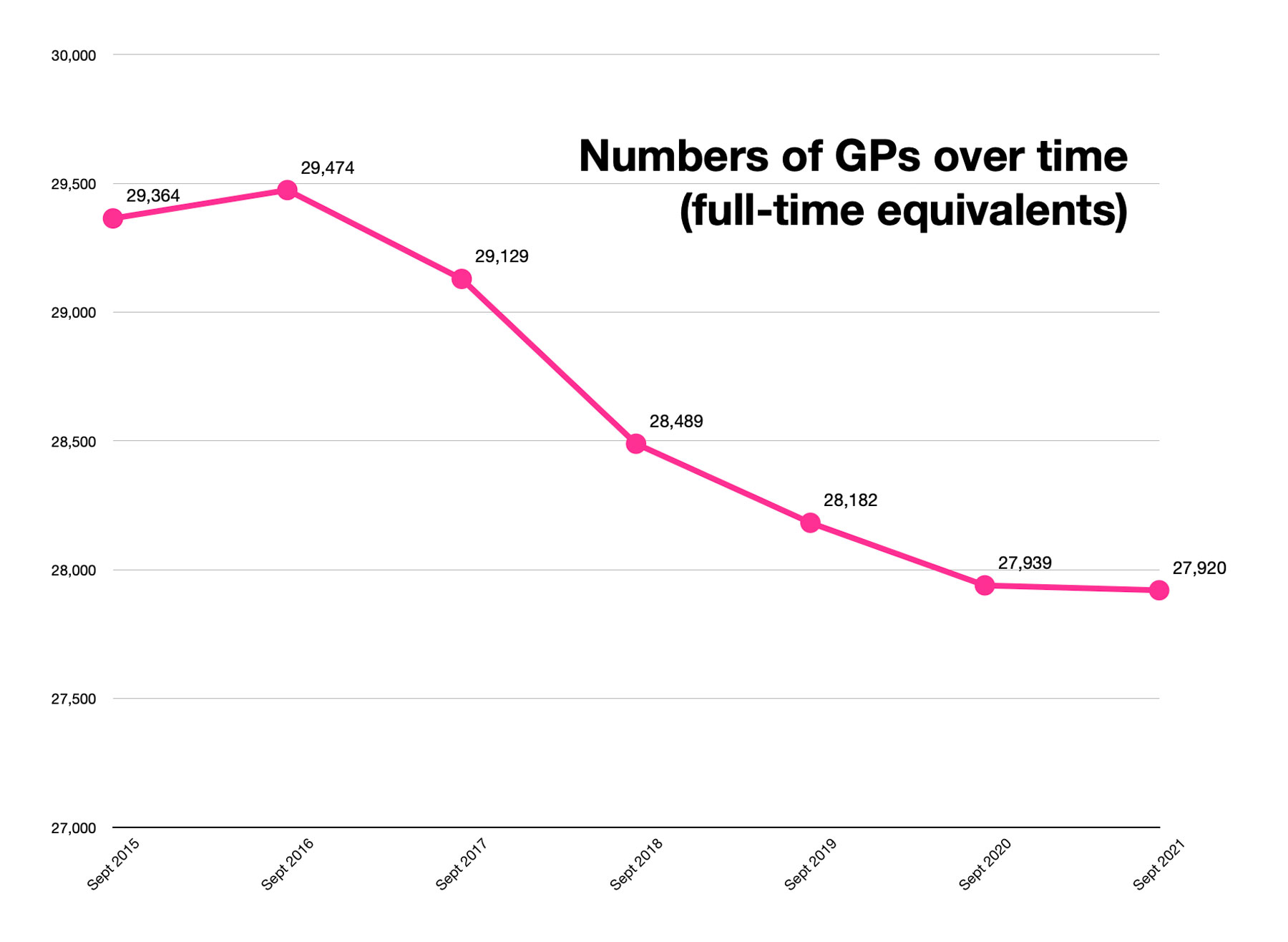
GP workload continues to increase whilst GP numbers continue to decrease. At the risk of sounding like a stuck record, it is still worth repeating some basic facts:
- The European Union of General Practitioners has stated that 25 consultations per day is a sustainable GP workload
- Even the government-endorsed Policy Exchange document At Your Service states that 28 patients is the safe daily limit
- GPs are now seeing an average of 37 patients per session, with 1 in ten GPs seeing 60 or more patients a day
- There are 1,565 fewer fully qualified full-time GPs in February 2022 compared to 2015 (NHS Digital official figures) - see graph below
- In February 2022 there were a total of 25.7 million appointments - this is 1 million more than in February 2020
- Beyond actual appointments numbers, GPs are also doing a huge amount of work behind the scenes, like referrals, dealing with results, medication requests (see Tip of the GP Iceberg infographic above)
- A single GP can easily make over 200 clinical decisions every day - a simple mistake in any one of which could spell disaster for patient and doctor alike
You may think, what is the point of mentioning this to you? Aren't these just excuses? No, actually the reason for letting you know these facts is that the shortage of GPs affects every one of us, as we are all patients and are registered with GPs and we all need care from a GP at some point in our lives. Not only that, but GPs and their teams make up most of the contacts in the NHS and their work helps to alleviate pressures on other parts of the NHS. Lack of GPs therefore affects the NHS and affects each and every one of us.
Simple maths shows that the whole system does not compute. Expressed as an equation, the formula is:
The GP service is under immense pressure, and GPs are very reasonably asking to work in a safe environment not only for their patients' benefit, but also for the sake of their own health and mental wellbeing.
If more is not done to improve the workload and working conditions that GPs and their teams find themselves in, the situation is only going to get worse - at the end of the day, GPs, as with other doctors and indeed other workers in the NHS, do not go on strike, they simply vote with their feet and retire, leave or emigrate.
What happens then, is that the existing and escalating workload lands on the shoulders of the reduced numbers of staff, increasing the pressure and significantly increasing risks to both staff and patients.
BMA: Safe Working in General Practice IVY.GS: Tip of the GP Iceberg GUARDIAN: GP numbers in England down every year GOV: Parliamentary answer on number of GPsGP CONTRACT IMPOSED UPON EXHAUSTED PROFESSION
Every year the GP contract is renegotiated and new terms discussed and mutually agreed. One would have thought that the work done by GPs and their teams over the last few years, including helping the country to emerge from the pandemic by administering most of the covid vaccinations to the population, would stand them in good stead in the eyes of the government. One would have thought the escalating workload and declining GP numbers as mentioned above would have been considered when looking at future GP work.
Despite all of the above, the government and NHSE have refused to discuss ideas and suggestions brought by GP leaders to support practices in the face of spiralling workload and costs, so that GPs can continue to deliver safe care to those who most desperately need it.
With their hollow and disingenuous words of support, the government has again shown no willingness to act decisively to support the profession, to provide resources to improve access, to promote safe working or to deal with backlog pressures in the context of an ongoing global pandemic that has impacted upon everyone.
As a result of the lack of agreement between the government and GP leaders on the contract, the government has again, for the third time since 2004, exploited a clause in the GP contract which allows it to impose the contract on GPs; a clause which was actually meant to be used only in the context of an extreme state of national emergency, such as war.
Ultimately, the thumbscrews continue to turn on NHS GPs and their hardworking and loyal teams, as the government pushes through its barely disguised agenda towards a salaried GP service and eventual privatisation of General Practice.
To give an example of the government's intransigence on the matter, let us consider GP working hours. Normal GP working hours are 8.00am to 6.30pm Monday to Friday (not 9-5 as reported widely in the media). The government has imposed changes to working hours to now include each weekday 6.30pm to 8.00pm and Saturday 9am to 5pm, so essentially an 8-8 service Monday to Friday, and 9-5 Saturday (the clear intention of this is to then impose Sunday working, and following that, force GPs to take back all out of hours care, but without the funding).
You may think how wonderful, that you would be able to access your GP any time 12 hours Monday to Friday and 8 hours at the weekend, but you already know how difficult it is to get an appointment during normal working hours now - there simply aren't enough GPs to manage normal working hours, let alone increase those hours by another 30%! To manage these hours, the existing workforce must be stretched even more thinly. Once again, it is a case of the maths not working, or more accurately, deliberately ignoring the maths.
If your intention was to push an already struggling service towards collapse, then clearly you would not listen to the actual workers in that service and their cries for help and support, no, you would actually impose a contract upon them which burdens the service with more and more work, more targets, longer opening hours, whilst promoting the idea that you were actually supporting the service and providing more choice and more service to patients whilst completely ignoring the fact that the service is haemorrhaging staff faster than they can be recruited.
All of this contract imposition comes at a time when the profession is completely exhausted and totally demoralised, having worked flat out for two years, and now currently seriously hampered by high rates of sickness caused by covid and stress, with all its resultant threats on safe practice.
General Practice remains in crisis and an imposed contract does nothing to help, but then the government knows this already.
IF WE HAVE NO APPOINTMENTS LEFT
The practical implication of all the above shenanigans, and the actual impact upon patients is clear. General Practice is a severely limited resource and by implication, there is a limit to our capacity. Although we want to help as many people as possible, we know our safe limits. Indeed, it is part of the duties of the doctor to not only recognise when one is out of one's depth, but to actively do something about it.
If we do not work safely and allow the work to simply pile up, then this will increase the risk of mistakes being made and patients coming to harm. The first person to be held responsible for this will be the clinician concerned, not the broken system that the clinician finds themselves in, not the government, not NHSE or any provider organisation. It will be that particular clinician in the dock. And that will not help anyone. Time and time again, this has been shown in various high profile cases with the GMC in the media.
Therefore if we have reached capacity for the day, this means that we are full. Once again, this is not about being awkward or obstructive, it is about managing our workload in a safe manner for the benefit of all patients and our staff. There is always help on hand should your problem be clinically urgent and there are always alternatives to seeing the GP as outlined in previous newsletters.
BMA: Pressures in general practice data analysis IVY.GS: Alternatives to the GPOther workers in the NHS
When talking about alternatives to the GP, this includes a number of other workers in the NHS.
We have made previous mention of the government's plan to expand the primary care workforce with new roles and staff, in order to not only reduce GP workload, but also to partially counter the severe shortage and reducing numbers of GPs.
Unfortunately progress in this area has not been as good as hoped, as there are still many thousands of different grades of staff that have not been recruited to positions in practices all over the country, and consequently hundreds of millions of pounds worth of funding has been left unclaimed and therefore lost to General Practice.
Whilst any plans to help address GP workload are more than welcome, we feel that the system put in place is not likely to be as successful as intended unless several very important issues are addressed:
- There needs to be flexibility in the funding streams, so that if staff positions are not filled, the funding is released to GP practices to enable them to directly employ staff or backfill with agency or locum staff. Currently, if positions are unfilled, the funding is lost completely to General Practice
- There needs to be significant cultural change away from the 'see your GP' (or 'ring your GP') mentality that has pervaded all of society as well as the minds of most other health professionals in the NHS for pretty much the last 30 years - perhaps the new phrase should be 'contact your GP team'
- There needs to be significant political change away from the single-minded emphasis on access to GPs, counting numbers of GP appointments, with no mention of these other workers in primary care
- There needs to be significant media change to move away from the incessant GP bashing, with no mention of these other workers, available and ready in primary care - it is hugely demoralising to everyone in the team
- For a proper team approach to work, there needs to be shared ownership and shared responsibility, not everything must or needs to come under the nose of a GP for the decision to be validated or confirmed - the reason for these additional roles is actually to relieve pressure on GPs, not to add to them
- There needs to be a massive national media and public health campaign to educate all patients and indeed other NHS workers, on the roles and responsibilities of these additional workers in primary care and to tell patients how they can self-refer to them, without recourse to speaking to our seeing a GP - this should not be left to individual GP practices to spread the word
Unfortunately, we do not see any significant or active work in any of the above areas, which will therefore limit the effectiveness of the whole enterprise.
Nevertheless, this does not mean that we at Ivy Grove will not try to introduce other members of the primary healthcare team, as this is in line with our longstanding philosophy of promoting self-care and self-referral to our patient population.
We have now started to add additional text and images to some of our self-referral pages, as in the examples shown above and right, to better illustrate to our patients the range of workers out there and their roles and responsibilities. We hope you find them useful.
IVY.GS: Index of services you can self-refer to without speaking or seeing a GP firstINTRODUCTION TO OUR HEALTH AND WELLBEING COACH
Whilst we are on the subject of other workers in the NHS, it is timely that we introduce one of our newest team members, Abbigail, our Health and Wellbeing Coach. Abbigail works full-time and is based in-house, working in close contact with the social prescribing service, to help support patients to identify their needs and achieve their goals. Here she says a little about herself:
Having grown up in Derbyshire, I moved away to study in Leeds before moving to the UAE to follow my passion for health and wellness. I chose to move back to the UK during the COVID-19 pandemic to return to university to study for a Masters degree, with a focus being on the relationship between Anxiety and Physical Activity. I am due to finish this in Sept 2022.
My hobbies include anything active, from weightlifting to marathons, I enjoy setting myself a challenge!
I am a Health and Wellbeing coach here at Ivy Grove Surgery. I can support patients to manage their health conditions, give them confidence and motivate them to become a healthier version of themselves. I look forward to meeting some of you very soon!
We are in the process of introducing some of our existing patients to Abbigail, however, any patient who feels they would benefit from Abbigail's help can self-refer to her if they so wish. To book an appointment with Abbigail, please ring the surgery, or visit our new Health and Wellbeing Coach page for more details.
IVY.GS: Health and Wellbeing CoachPlease also see below the inspiring story of Scott, one of our patients, who has overcome his own issues in a bid to become healthier, and also see our page for the social prescriber service:
Scott's Running Madness IVY.GS: Social prescribing serviceJOB VACANCIES
We currently have a number of job vacancies available. If you already work in the NHS or even if you don't have the experience, but think you meet our various person specifications, and you are looking to join a friendly, forward-thinking team then please take a look at our jobs page - on the admin side we are looking for a practice business manager, reception manager and receptionists, and in terms of clinical staff, we are looking for a practice nurse and a six session salaried doctor.
Anyone who is a regular reader will already know, but to those that don't, let us be honest. It is no secret that times are tough in General Practice, with increased workload and demand, with everyone wanting a piece of you; there's no doubt that it's as busy everywhere in the NHS with no let up at the moment. But if you would like to join a GP surgery that recognises this pressure and one that actively does something about it to make things easier, one that looks after its staff and consider them as part of its 'family', so that they can all work together in the best interests of its patients, then look no further.
If you know someone who works in the NHS and who is looking for a new challenge in general practice, please feel free to share our jobs page link with them. We welcome all interest and are more than happy to accommodate informal visits from prospective applicants.
IVY.GS: Jobs page IVY.GS: Practice manager job IVY.GS: Practice nurse job IVY.GS: Patient care advisor / receptionist job IVY.GS: Reception manager job IVY.GS: Salaried doctorVIDEO CONSULTATIONS
As IT-based solutions for General Practice relentlessly march on, you might find that your GP suggests a video consultation using your camera-enabled smartphone. Whilst this might feel very daunting for some, it is actually quite easy.
Whilst most remote consultations can be carried out by phone (along with photos of visible conditions where necessary), there are certain circumstances where video consultations have proven useful. For instance, to quickly eyeball a sick child, or, in the case of patients on the palliative care or end-of-life register, to perform a remote review without the risk of putting an already vulnerable patient at risk by a health professional visiting and bringing covid with them.
Our video consultation solution is provided by the same company that provides our text message solution, AccuRx. Here we provide the link to the instruction page from AccuRx that describes the process for connecting via video to your GP.
Please try not to worry if your clinician suggests a video consultation. They would only suggest this if they feel you are willing and able to accept a video call and they will always talk you through the process, step by step. Ultimately, should video consultation fail, we can always revert back to telephone or face-to-face consultation by traditional methods.
ACCURX: My clinician has sent me a video linkPRIVATE PROVIDER REQUESTS
We are often asked by private providers, e.g., consultants from private hospitals, to do certain investigations and/or prescribe specific medication for patients.
All our patients should be aware that complying with these requests is not within the scope of NHS GP services, which according to the GP contract, are defined as services which are delivered in the manner determined by the GP in discussion with the patient.
Whilst it might sometimes appear to be the case, GPs are actually not here to serve other workers, private or otherwise, in performing jobs for them. In this case, private providers, when they see you, are responsible for carrying out their own investigations, actioning the results arising out of those investigations and also providing treatment where necessary.
Therefore a GP will carry out investigations and prescribe medication for a patient where it is necessary for the GP’s care of the patient and the GP is the responsible doctor. This is clearly not the case where a patient is under the care of or receiving active treatment from a private provider.
In short, the responsibility for carrying out such tests and prescribing medication lies with the private provider.
The official BMA guidance is quoted below:
We therefore respectfully ask that if any patient is in this situation, to revert back to their private provider for the completion of such investigations or treatments. We are more than happy to provide copies of medical records to any patient to facilitate information transfer for any necessary ongoing intervention from the private provider.
As touched upon above, we must remind all patients that the responsibility for following up any test result lies with the clinician who ordered the test. This is the case whether the test was requested either on the NHS or privately.
Therefore, if you are needing to chase up or follow-up a result of a test organised by the hospital, please contact the secretary of the hospital consultant in the first instance. We have a page set up to inform our patients of this.
BMA: Private provider requests for investigations under the NHS BMA: Duty of care when test results and drugs are ordered by secondary care IVY.GS: Hospital CarePRIVATE FEES FOR NON-NHS WORK
The NHS provides healthcare to most people free of charge, but some fees have existed since the early days of the NHS, e.g., prescription charges. GPs are self-employed and are contracted by the government to provide medical care and this is free at the point of contact.
Work which is not part of NHS work is not covered in this contract. Examples include insurance reports, pre-employment medicals, reports for fitness to work or drive and holiday cancellation reports.
It might surprise many, but the fact is NHS GPs are not obliged to carry out any non-NHS work, however, in order to help our patients, we may agree to do such work, but it will be charged for in line with our private fees. Please check our waiting room noticeboard or our website for details of our private fees.
There are some types of non-NHS work that we do not carry out at all, regardless of any fee. Examples include: character references, housing letters, dieting approval confirmation, fitness to parachute forms, testamentary (wills) capacity. Please see our Forms and Letters Policy for further details and reasons.
In order to assist patients in making their own representation for non-NHS work that we do not carry out, we are more than happy to provide a summary printout of your medical record free of charge for you to use and/or send to whomever necessary.
IVY.GS: Private Fees IVY.GS: Forms and Letters PolicyHOSPITAL WAITING TIMES
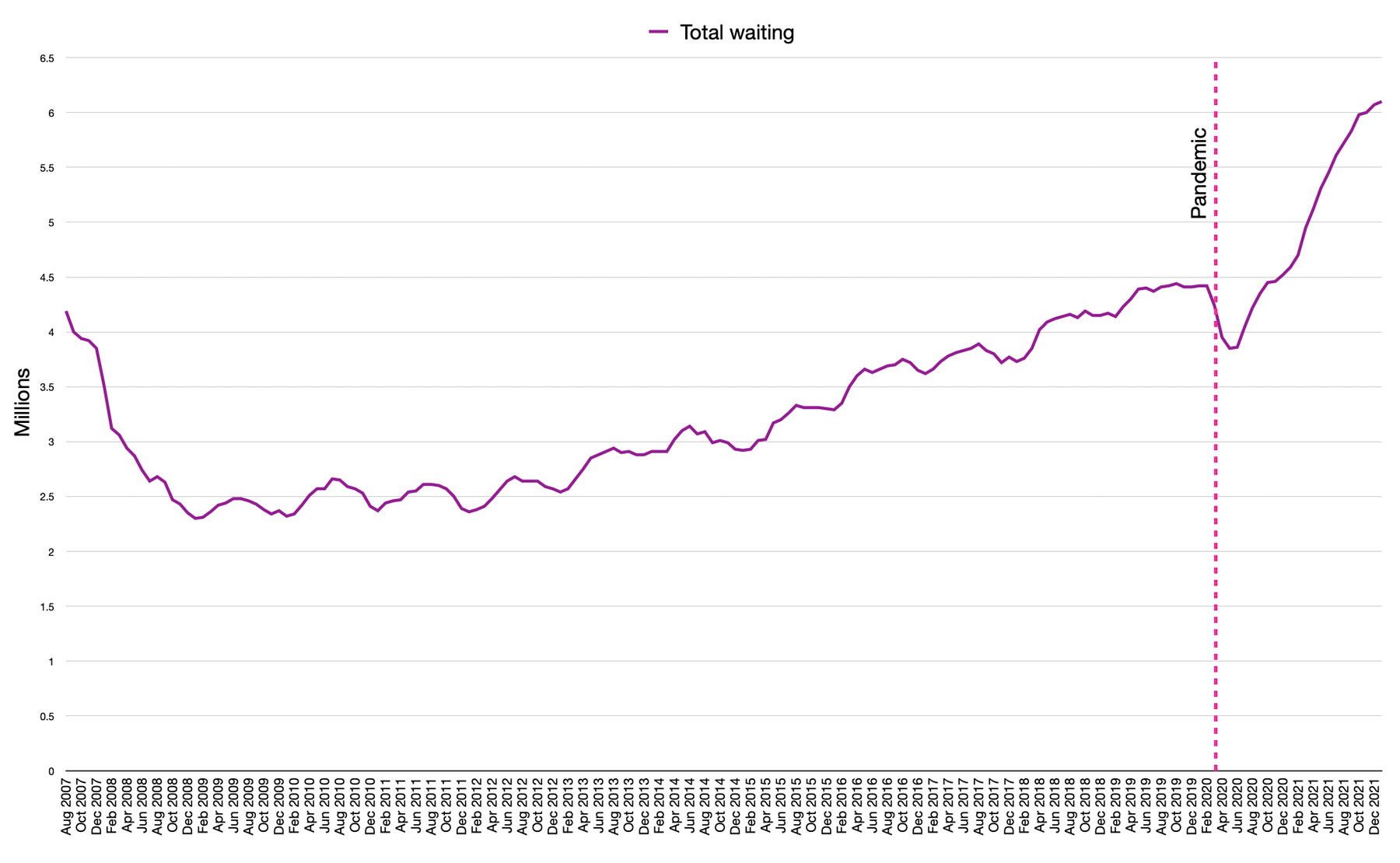
Prior to the pandemic, there were 4.4 million people waiting for hospital care. As of January 2022, official NHS figures now show a record 6.1 million people waiting for treatment. This is a combination of patients already on a waiting list for treatment, patients who have had procedures cancelled, or referrals delayed, or even refused due to lack of capacity (see graph below right).
It will take years to clear the backlog. The ongoing need for infection prevention control measures and workforce shortages mean it will take even longer to work through the backlog as demand continues to rise. In addition the hospital will always be giving priority to the more clinically urgent and cancer cases, where time may be a factor that affects outcomes.
We are being frequently contacted by patients who are already waiting for hospital care, with the expectation that we will be able to bring forward their hospital follow-up appointment. We kindly ask that any patient in this situation and who finds that their condition is actively worsening whilst waiting, to try and get in touch with the hospital secretary first. We do not have any special hotline numbers with the hospital, and the numbers you have on your outpatient letters are the same as the ones available to us.
Unfortunately we do not have the capacity to ring the hospital on patients' behalf as this would not only tie up our already busy phone lines but also tie up our staff who need to process letters, results and other tasks.
If you ring about your follow-up appointment and are told by the hospital secretary that you must speak to the GP for a letter to speed on your appointment, please note that this is incorrect advice. For those patients who are already waiting to be reviewed for a condition that the hospital already knows about (follow-up outpatient appointment), the hospital is obliged to consider your own representations on the matter. For patients who have yet to be assessed by the hospital for their new condition (new outpatient appointment) and who are actually getting worse, please contact us.
If your issue is simply that you think you are just waiting too long, unfortunately, very many people are in the same situation (see graph), and there consequently will be very little that can be done about this.
We have created two pages on our website to provide a little information on the situation of hospital care (tests, results, procedures, operation wait) or expediting appointments, and we also include a link to BMA official information.
IVY.GS: Expediting an appointment IVY.GS: Hospital care BMA: NHS backlog data analysisSCOTT'S RUNNING MADNESS
Now for an inspirational message from one of Dr Smith's patients - please consider backing for his amazing efforts in support of good causes
Hi. My name is Scott and I live with multiple conditions that mostly can’t be seen and aren’t always understood!
To give a bit of information and clarity on this, the conditions I live with are severe depression, social anxiety, autism and Parkinson’s disease. I am 46 years old. Despite all of this, and like most other people, on the outside I appear to live a normal and relatively boring life – but underneath that outer persona it's far from that, so please read on and let me explain.
This is taking a lot to write but here goes. In a nutshell, 26 years ago I suffered some traumatic treatment from a very abusive relationship that led me to becoming 'unhappy and down' but then as time went on I became more and more reclusive and further 'down' to the point my employer noticed and sought out help for me through medical professionals. I was diagnosed with severe depression and advised to go to hospital for help and support.
That wasn’t possible for me as I was faced by the 'you’re supposed to be a man so get over it' attitude. I continued to try and work through it because 'mental health isn’t a thing for men' – well, actually it is, as I found out years later, yes, years later. I’m not going into huge details as I want this to remain private, but let’s just say I am still needing help and support over 20 years later!
This continues to be one of the reasons for my social anxiety along with my autism, and now more so with my recent diagnosis of Parkinson’s Disease (PD). My PD was diagnosed just over a year ago. I get the well-known tremors, but these are only a really small part of the condition - there are hundreds of other aspects that unless you live with, or live with someone who has, PD you may never know or even think about.
This is everything from forgetting what you were doing whilst doing the actual activity, to daily activities taking much longer than you think. There is medication for PD, but there is no cure and it is also degenerative, so will get worse over time. It is very unusual to be diagnosed with it as young as I was.
So what am I doing about all this? Staying at home feeling sorry for myself and wallowing in self-pity? – sounds nice but NO! With the help and support of staff from Ivy Grove Surgery, especially Dr Smith (yes I am naming you) I am living my life.
I do this through a passion for running and getting outside and meeting the challenges head on. I use the time I run (both with two brilliant local running groups and on my own) to gain what I call ‘headspace’, this is my time to put all of life’s negativity into a ball and use it to empower me! Sounds a bit nerdy but it really does help!
Spending the time in the open, and the feeling of achievement at completing a run no matter how long or short is amazing, the sense that I can slow the progression of the Parkinson’s due to the physical activity, the way you can't stay angry or upset when running (this has been scientifically proven and I can confirm through personal experience) is amazing.
All you need is a good pair of trainers, T-shirt and shorts (ladies, a supportive undergarment would be advisable as well!) and somewhere safe to go. As such last year, I ran quite a lot and at a steady pace and this started to help me a bit more especially when I ran a race and got my first medal, runners bling!
So this year I have challenged myself to do more, a lot more - I am running an event every month this year to raise money for charity, I don’t just mean small events but some really big events. I have NEVER run more than a 10km race (6.2miles) so this year I am entering at a 5 mile cross country race, at least two half marathons 13 miles (21km), a 20 mile (32km) race, one marathon 26 miles (42km) and one race of 100km (62.5miles)! I will also be doing do the local Parkrun every week.
Now that I have opened up my soul a bit to you, I was hoping you would be gracious enough to consider supporting me in this by donating to my donation page. All the monies raised will be split between Parkinson’s UK for their research and support, and also the Specialist Rehab Unit in Derby Florence Nightingale Hospital who are not only a centre of excellence for PD but also support patients and families with multiple neurological conditions from both accidents and illness.
If you can help, even just a little bit, I thank you in advance. But more than that I hope this articles helps to raise people's understanding that just because people may seem okay they may not be and that it really is 'okay not to be okay'! I hope I may have also inspired someone reading this to challenge themselves and meet their goals!
This is my donation link and I will thank you all individually!
Scott's Running Madness!There will be a pot called Scott’s Running Madness in the surgery if you would like to donate that way and a sponsor form for your name so I can thank you that way.
Many thanks for reading!
Scott
For further information on Parkinson's disease, running, health and fitness, please see the links below:
Parkinson's UK NHS: Parkinson's disease Parkrun Live Life Better Derbyshire Active Derbyshire NHS: Couch to 5KPatients may also find the following links helpful:
IVY.GS: Mental health support page IVY.GS: Counselling page IVY.GS: Health and wellbeing coach pagePLEASE USE THE MEDICINES ORDER LINE (MOL)
Just a reminder to all our patients who are taking repeat medications, that you can now use the Medicines Order Line (MOL) to order your repeat prescription requests.
Ordering your repeat prescription involves a quick and simple telephone call to a dedicated person who will have time to answer any queries you may have about your repeat prescription and discuss your medication requirements.
The MOL opening hours are Monday to Friday between 8am and 4pm.
Download MOL leaflet Ring 01246 942751 for the MOLLATEST POSITIVE FEEDBACK RECEIVED
Continued thanks to those who are still sending in messages of support and for your impromptu gifts. We publish these comments to share with the rest of our patient population in the same way that we share all similar messages with the rest of our team: to share in goodwill, positivity and hope during such difficult times.
To Dr Axten and the Nurses and Staff at Ivy Grove Surgery, many thanks for your prompt and no-nonsense approach to my recent medical incident – S
I can't thank Dr Wong and Sarah (reception) both enough for all the help that they have given last week – JB
Ivy Grove, Everyone so helpful (as always) and I am very grateful - a huge thank you to you (Enid), Tomorrow always settles, Care from – ZR
Thank you for your kind consideration and the help provided – WS
I would like to thank Dr Francis for the excellent phone call to follow up medicine enquiry. He was informative and put my mind at rest about the medication. Very happy patient – JR
Thank you so much for the reassurance and kind and efficient service I received this morning when visiting the surgery, especially from Michelle and subsequently Dr Wong in relation to my mum. The prompt attention she received today has helped relieve mum's anxieties about her current problem and I’m sure prevented unnecessary hospitalisation. Please never underestimate the difference you make, a huge thank you for all you do especially in these very difficult times. Please pass on my gratitude – AR
Thank you to the whole team for all your hard work – JW
To the staff at Ivy Grove Surgery, thank you for keeping my family healthy this year and for being there for us when we have needed your help, with love and thanks – KD
To all the staff at Ivy Grove Surgery, Thank you so much for your continued care to all patients especially during the past 2 years - a very difficult time for everyone, you've all done a great job, kind regards – DP
I want everyone to know how helpful and thoughtful Vanessa was last week – AP
DISCLAIMER
We know not everyone shares in the sentiments that we present here. Whilst we always accept constructive criticism and feedback on all our services and we do use these to help change processes and improve our services, we do receive a few messages on our feedback form from patients who are clearly ranting against GPs and the politically driven system that they find themselves in. These negative messages are actually very few in number when compared to the overwhelming number of positive feedback messages we receive.
Whilst we note their contents, we would prefer not to share these as they would not help anybody and would simply bring everyone down at a time when things are horrendously difficult for us all, both staff and patients alike. Ultimately, we are all trying to do our best in a system that is clearly struggling.
In any case, we get more than enough 'GP bashing' in the media, and we would never dream of publishing or promoting such links in any of our newsletters. So please excuse us when we apply the same principles to any other messages that are of the same ilk.
Please also bear in mind that the feedback form on the website is not intended as a formal communication channel with the practice, nor to provide any clinical advice, that the inbox is not monitored regularly with the consequent risk of significant delay in us receiving your message, that it is not 100% secure for confidential information and that finally, by using it, you acknowledge that you do not need a response from us.
If you actually have a formal complaint about our services, where we have clearly made a mistake in our care for you, or you need a formal response to your feedback, please do write to us.
FINALLY...
Please continue to keep safe whilst we start to come through to the other side of an awful few years. We hope that things will only get better!
Kind regards
Ivy Grove Surgery
Written by Dr M. Wong
© Dr Michael Wong 2022