Latest News Update 19.4
May 27, 2021
Dear Patients
This is our latest news update following on from our last one in April. Previous updates issued throughout the course of the pandemic can be found here.
COMMENTARY ON OUR OPEN LETTER
It's been an interesting month. Our monthly news update, which is usually read by about 3,500 to 4,000 of you whenever we post it out, actually went viral with hundreds of thousands of views of our open letter and prompting lots of discussion about General Practice as well as some abuse. Our website has served thousands of downloads of the letter and other materials over the last month.
Notwithstanding the statement that we have already published, we would like to make some comments about our letter, so we will start by thanking our patients who have supported us throughout this last year with their patience, understanding and compassion. We will continue to strive to provide you all with the best care that we can.
Open Letter One page summary Media statementIncreased demand from all sources is the problem
We need to emphasise that, although we introduced our letter with online consultations, it is clear that they were just the last straw that broke the camel's back. The online consultation service, with its unrestricted access, has contributed to an interconnected and complex system of increased demand and huge workload that we have experienced over the last year or so.
So back to the letter. On the one hand, we had a very vocal group of random people declaring that the letter was the rant of a burnt out team who didn't seem to care for its patients. This was coupled with, we might add, some anonymous trolls who did not have the courage to put their names on correspondence to us. And on the other hand, we were overwhelmed with hundreds of positive messages of support from other GP surgeries and health professionals all around the country (and indeed abroad too) whose own experiences resonated with ours. We have 10 pages of A4 full of positive feedback so far.
So strong was the outpouring of support and solidarity from General Practice, that, on request, we have shared our document widely with other GP surgeries nationwide, so we expect to see similar initiatives elsewhere in the future.
And in the middle, we have had our own patients, presenting no negative feedback at all on the changes we have made, and indeed a select few of our own patients valiantly defending us on social media against the bitter vitriol with some sterling support, very much appreciated and very kindly received, a heartfelt thank you to each of you.
I read this yesterday as a parent of a patient with Ivy Grove. They are an exceptional practice, throughout covid have been able to be seen or telephone call. I can see how they are a victim of their success and I understand the letter. – AD
Clearly primary care has faced it's challenges during the #COVID19 pandemic but despite the haters of @IvyGroveSurgery, I can honestly say my family have been looked after extremely well in the last 12 months. Phone calls mostly but F2F when clinically needed. Happy days. – AH
I think you have all done an amazing job through these unprecedented times. I have received A* treatment from my GP and am eternally grateful. – DS
We can also very happily report that all the patients who have had contact with us since the letter and since our changes, are very grateful for the opportunity to speak with their GPs when seeking our help and we have not had a single patient lament the loss of online consultations. This we feel is rather telling.
Just a reminder of the changes: below, you will see links to find the help you need; if you need our help, don't hesitate to give us a call and speak with us. We will always assess you remotely to begin with, and then bring you in to see us face-to-face where this is clinically necessary.
Self-care Self-refer Symptom checker Get the right help Help during covid Mental health support Ring us Ring 111 NHS 111 online NHS Health A-ZSince its inception, General Practice has always been about having regular conversations with patients, either face-to-face, and significantly, even pre-covid, by telephone, and we are not sure that the move towards a more transactional-based service is always going to be in the best interests of patient and clinician alike.
We all form part of the system of General Practice
We can understand the comments that the letter could be seen as patient-blaming; whilst we do not agree that the letter is of that nature, nor was it intended to be interpreted that way, we must say that patients are part of the system, in the same way that we GPs are part of the system and the government/NHS England (NHSE) are part of the system. One therefore cannot discuss General Practice, nor the expectations that any patient has of General Practice without mentioning the actions and behaviours of patients.
We have heard the argument that we should have addressed our concerns to the government. Those of you that know us, will know that we have attempted to do so, repeatedly and without success. We have previously written to the then Prime Minister, the then Health Secretary, and met with our local MP, along with subsequent additional invites to discuss the state of General Practice, all without success. We have also in the past written to our GP leaders clamouring for action and change.
We have previously been in correspondence with NHSE and its departments on a variety of issues, again without success [the last time we tried this was to lobby, along with other GP surgeries, for our hardworking staff to be able to finish slightly early on Christmas Eve (at 4pm instead of 6.30pm), given that it is, and always has been, an exceptionally quiet time of year with everyone busy doing last-minute shopping or settling down with family – needless to say our reasonable request fell on deaf ears, rejected by the very staff who would have already gone home at lunchtime that day. Ironically, having given up pushing every year for this goodwill gesture, it was rather surprisingly granted last year after some campaigning from our LMC (Local Medical Committee)].
It also appears that NHSE's role is simply to rubber-stamp, without any degree of critical appraisal, the government's relentless drive towards increased access, increased expectation, increased demand, with their consequences upon workload, without tackling any of the genuine issues on the frontline, examples such as recruitment and retention, working conditions, unnecessary administration and red tape, tedious and overbearing micromanagement, onerous over-regulation and inspection regimes, misplaced accountability and responsibility, reduced funding, poor IT support, nor taking any steps towards addressing the significant impact of societal and cultural change upon General Practice, and above all, not investing in it or its future.
From a patient perspective, ease of access and wonderful convenience might be very welcome, but the end result of prioritising access and convenience above all else means that lip service is paid to the other key assets of General Practice such as patient-centred holistic care and long-term relationships built on continuity.
These key values are what makes General Practice safe and effective and lend weight to it being hailed as the 'jewel in the crown of the NHS'. These are also the things that patients and GPs themselves both value very highly, but are discussed the least (perhaps because they are implicity asssumed to be present in each interaction), until something goes drastically wrong, when the significance of their absence in the turn of events becomes markedly clear. It is our view that patient safety must alway trump patient convenience.
Relentless push towards access and convenience without matching investment risks patient safety
Whether it is as a result of wilful actions or ignorance, or more likely, a lot of both, we can quite honestly say, that despite its knowledge of what is happening in General Practice, there has been no useful initiative from government in the last 15-20 years that has been specifically aimed at or been genuinely successful at relieving pressure on the frontline or improving the toxic environment that GPs and their staff find themselves in on a daily basis. Indeed the direction of travel has always been to increase pressure on already severely strained services. All we hear of are deliberate moves to increase access and availability, to increase convenience, to increase administration and control. One could argue about the intentions of such a single-minded drive, however that is for another time.
But what about GPs themselves? GPs and their staff are the ones supporting every patient request, every contact from other outside agencies, every diktat from government and NHSE, they are behind every action that you experience as a user of General Practice. GPs and their staff are exhausted, tired and ground down with demand for their services from every angle. But we know that a great many of them do not say anything publicly about what they are experiencing every day. One might wonder why this is.
It is clear to us, from the feedback we have received, that many GPs are living in a climate of fear, fearful of putting their heads above the parapet [those words have been used multiple times in feedback to us], fearful of saying anything that could lose them patients and hence income, fearful of reprisal from the government or its agencies, fearful of the multitude of regulators that scrutinise our every move, fearful of the spotlight or media backlash. We also know that many are simply tired of fighting and after their soul-destroying days, utterly demoralised and having neither the energy nor motivation to be able to mount a useful response to what is facing them.
A climate of fear and sheer exhaustion prevents GPs from vocalising their concerns
Unfortunately for all of us, this silence will mean that most people will remain ignorant of the precarious state of General Practice and what is happening behind the scenes. All people will know is that it's difficult to book an appointment or get in touch with the GP (perhaps contributing to the widely-held belief that GPs aren't actually doing anything very much and the consequent increasing levels of abuse), but behind every engaged tone or exasperated voice you hear there is actually a story; you might not hear about it, or want to hear about it, but it is happening all the same.
So we have a vicious triad of expectant and increasingly demanding patients, increasingly dejected but silent GPs and an increasingly intransigent government. This does not make for a healthy General Practice. Given we appear to have no influence on government policy to change things for the better, all we can do is either change ourselves and/or change our patients' behaviour. As a practice that is more than ready to make changes to improve matters for our patients and our staff, and given that our practice philosophy has always involved being open and honest with our patients, with an emphasis on working together to improve services through involvement and education, our letter of explanation was just one example over the course of many years.
Demand and workload threaten patient safety
Whichever side you fall on, we make it absolutely clear that an open and honest debate, on demand and workload in general practice and a discussion about the expectations of what can realistically be achieved in the current climate, is well overdue. Those of you who have read our letter fully and clearly understood the complexity behind General Practice, and have appreciated the weight of feeling behind it, will have realised that ultimately, we come from a position that the current escalating demand and workload we face in General Practice has the potential to adversely affect patient safety and staff health.
If all you saw from our letter is concern over patients being upset, or think that privileged doctors are giving a patronising overlong lecture, then we apologise for not making this clearer: excessive, unrealistic, increasing demand leads to unsafe workloads that threaten patient safety and the health of GP surgery staff.
Unchecked demand leads to unsafe workloads that threaten patient safety and staff health
This is vitally important, because we are all patients in this NHS and we will all need GPs and their staff at some point in our lives and all of us need safe care. As we grow older, or get sick, we need to know that there will be a safe and effective General Practice that we can turn to, to help us, to treat us and to advocate for us. It is in all our interests to preserve General Practice for ourselves and future generations.
The GP service in perspective
As an aside, it might interest people to know that your GP surgery receives the princely sum of £96.78 to provide care for one patient for one year*. This amount is fixed. It doesn't matter if you consult with us once, twice, a dozen times or a hundred times [we have some patients consulting with us 100+ times a year] . We don't get any more funding for each additional consultation we have with you.
From this single figure, we must pay all our bills to keep the business running such as heat, lighting, staff wages, equipment and the partners get what's left. We find that most people consult with us around 7.5 times a year on average [this is up from 3 times a year in the early 2000s and 6 times a year about 5-6 years ago]. Quick calculations with the £96.78 funding shows that things are somewhat tight to put it mildly.
Each of the consultations you have with us in a year is equivalent to providing us with around £13 of funding
A typical business offering 'convenience' and 'access' and 'ease of use' would be able to generate increased income through more customers/footfall, therefore enabling it to employ more staff, to offer more services, to scale up to meet demand, and encourage even more attendance, higher turnover, more profit.
You can see that this actually doesn't work for us as we cannot easily hire more staff from our fixed amount of funding to cope with increased demand as this would make the business unviable - this 'all you can eat' model of General Practice has remained unchanged for decades, even though demand has increased many times over.
Although technically we are self-employed and subcontract our services to the NHS, in reality, we have a monopoly employer who can turn the thumbscrews, decide what they want to pay us and change our contract at will [the GP 'contract' has a clause in it which enables the government to make unilateral changes to it without agreement; meant to be used in times of national crisis, like war, but exploited twice already just to impose harsher working conditions].
To put this £96.78 into perspective, the cost to the NHS of an attendance at A+E is £150 each visit and the cost to the NHS of a hospital stay is £400 each night. The cost to the NHS for unlimited contacts with your GP or nurse is £97 per year; your GP surgery provides you with all the care that you need for just 37p per day. If you can understand the significance of these figures, you will come to understand not only the sheer value for money that General Practice provides, but also the pressure that General Practice is under.
Compared to this £97 annual NHS funding figure, the cost for one (ONE) consultation with a private GP provider starts from £50-£100 and visits can cost anything up to £300. So you can see with the annual funding that we get for your care, it should accommodate only one or at most two surgery consultations each year.
Your GP surgery receives just 37p per day to provide you with unlimited care, compared with the cost of one A+E visit at £150, or one night's hospital stay at £400
But, although money is clearly important, we are not really talking about money here. We actually want more colleagues, more resources, more trust, more support, more patient education, more public health, more self-care, more self-help, more resilience in the population, more societal improvements, along with less red tape, less administration, less micromanagement, less tickbox medicine, less interference, less negative press. Any of these things would do a tremendous amount to help improve General Practice.
Ultimately, what we are talking about is demand and workload, that has been steadily increasing in General Practice over many years.
What we are seeing in General Practice might be a reflection of the movements we are seeing in healthcare generally, which are overall quite worrying. It's too much to go into right now (perhaps another write-up for another time!), but in short, there is a real risk of over-medicalising everything that happens in life, of a deepening and disturbing dependency on healthcare, of actively encouraging not only an increased anxiety about our bodies and our minds but also at the same time, fostering an increasing lack of ownership and responsibility for them and then, of offering 'solutions' without providing the resources to match. And finally, of vilifying those NHS workers who then fail to deliver on the promises that they had no chance of meeting in the first place.
By the way, in outlining the above, we are not talking about hypochondriasis. We are talking about trends in society that do not actually make us, as a society, any healthier. In fact, such things disempower patients, and are actually a sickness in their own right. Do we ever discuss these important issues? No, we do not because they might be considered unpalatable to hear or not politically correct to air. But they are still important issues nevertheless.
Everything that is happening now has the potential to risk General Practice and its future and the safety of patients, and at Ivy Grove Surgery, we feel we have a duty to let everyone know the truth. Indeed, you could call it a form of whistleblowing. Whistleblowing on the unproven policies of government, an account of the unintended (or possibly intended) consequences of deliberate over-promotion of a troubled service whilst simultaneously underinvesting in it.
Ultimately, we have told no lies in our letter and regardless of your view on patient-blaming, tone, messaging, length, presentation or otherwise, all we have done is that we have reflected on our service as honestly as we can and provided you with our true observations on our day to day work, along with suggestions about what you can all do to help.
Healthcare must always be a partnership
This brings us to the subject on what patients can do to help. In our open letter, we suggested that healthcare should be a partnership between patient and carer, and that all patients should take some responsibility for their own health. We are astounded to find such fundamental principles are somehow deeply offensive to many, and are reported to be completely at odds with the provision of healthcare.
We completely disagree. We maintain that healthcare must be a partnership for it to work effectively and efficiently and as part of that partnership we consider it entirely reasonable to ask patients to do what they can to look after themselves, to stay healthy as best they can and to consider how they might access the right help, from the right professional, and at the right time.
We believe the attitude of being aware of your body and mind, of looking after your own health and of being healthy and of knowing what to do when things are not right, starts from childhood, from parenting, from schooling and education, from rigorous public health campaigns, and this learning should continue right through life. It should not be left until you are sick and your automatic course of action is to then contact the GP.
All we hear in the media are phrases such as 'GPs must do more to…, or 'GPs once again fail to…' or 'too many GPs…' (if you search these terms, you will find many examples), but never do we hear any words or phrases that suggest that a prior discussion, a partnership, a negotiation, or a shared responsibility would be more appropriate to help bridge the gap between demand and supply.
We hear much about patients' poor experiences with their GPs, much about what GPs should do but have failed to do, but nothing at all about what GPs are actually already doing, nothing at all about what GPs can reasonably do, and nothing at all about the consequences of GPs having to do too much.
At this surgery, we have always tried to address this issue of partnership by advising you on how to look after yourselves and how to work with our service in order to get the best care.
Make the most of your GP Did you know...? Day in the life of...General Practice as it stands is unsustainable
The doctors at Ivy Grove Surgery together have over a century of experience in the NHS. In recent years we have lost an additional century of experience from older GPs retiring, mostly before their due time, or younger ones leaving General Practice or indeed, medicine, altogether. And we are certainly not soft; we actually consider ourselves to be quite a resilient bunch, but we can honestly tell you that the relentless demand that General Practice as a whole is facing, the huge workload, the expectations placed upon the service, are all making General Practice unsustainable.
GPs have seen more patients than ever since the entire history of the NHS
NHS England's own official figures from the month of March 2021 show that GPs have seen the greatest number of patients since records began, and indeed ever since the entire history of the NHS, with half of contacts taking place face-to-face. Figures also show that GPs remain a limited resource, indeed they are a diminishing resource, therefore simple maths show that this simply cannot continue.
As a kind of thought experiment (bear with us here), think about a free* service that might be available to you, doesn't matter what the service would be, as long as it's free. Just as an example, say it's retail (the government does like to apply a retail style approach upon healthcare, with ratings, accessibility, convenience, so quite apt). So, say the nature of this free retail service would be to provide you with free groceries whenever you wanted, but at the start, only during office hours. It gets popular quite quickly.
Those that work can't always access the retailer during office hours. So now the management board of the retail service wants it to open more hours, at evenings, and at weekends, which it does, after some resistance. Very quickly, and as expected, the free service is immensely popular. The board is thinking it might actually want the service to open 24 hours a day, 7 days a week, but hasn't got round to implementing that yet but definitely will come back to that later.
Anyway, the service is already experiencing huge demand with the customers expecting all their free groceries very frequently, but its staff are struggling to meet the demand and are under huge stress now. They're making mistakes, getting the wrong groceries picked, missing orders completely, rushing orders through, the groceries provided are of poorer quality and the customers are generally not satisfied and levels of abuse and complaints against the staff increase.
The management board demands that the retailer must continue regardless. It must offer not only a high quality service, but also one that is highly responsive and above all, it must be free at all times for the convenience of the customer, for them to access at any time of day or night (even though the staff that work for it only work during office hours). What does the retailer do? Demand is escalating and is damaging the quality of the service it can provide.
In order to continue the free service, the retailer might then need to limit the amount of times you could claim your free groceries, or perhaps it might need to limit the amount of free groceries you could get each time, or if it was met with such high demand, there would have to be an increasingly long wait before you could get to the front of the long queue to get your free groceries. If demand continued to escalate, the free service might have to charge a token fee to just make people reflect before getting their free groceries, or if the free service was completely overwhelmed, it would have to shut.
Not sure about you but we don't want General Practice to shut (we need it in our dotage, remember). For 'shut', read 'fail'. But as mentioned in our open letter, General Practice is already failing in various parts of the country, with 800 GP surgeries having closed their doors permanently in the last 8 years - you never used to hear about GP surgeries closing, but now two closing per week is the norm. It's not scaremongering to say, because it's true, if General Practice collapses, along with its capacity to assess over 1 million patients a day, you can be absolutely certain that the entire NHS will collapse shortly after.
If General Practice fails, the NHS as a whole fails
We therefore welcome open discussion and debate on the state of General Practice, and we welcome positive change for the better. If our letter went a little way to start some debate then we would be pleased. What we do not welcome is knee-jerk policy change based on newspaper soundbites or malicious media campaigns centred on the complete and utter falsehood that GP surgeries have been closed, or that GPs are lazy or obstructive, or that they are not seeing patients or deliberately hiding away behind their desks or behind their phones.
The irony behind these lies seems to have been utterly lost on those spreading them. If GP surgeries really are closed, with GPs not working, then something else must be occupying all their phone lines all day. If GPs are rubbish, and not worth seeing, then they do seem to be unjustifiably popular for them to be kept at their desks for 11-12 hours a day. And if waiting rooms are just empty, it must mean that the hundreds and hundreds of daily documents, results, tasks, notes and callbacks must be tackling themselves and filing themselves away. And if lazy GPs and their staff haven't been up to anything much at all lately, then the country must have vaccinated itself out of the pandemic*. Face-to-face.
To believe such damaging lies is a cruel betrayal of the hard work and dedication of all the surgery staff, from verbally abused receptionist, to harried secretary, through to exhausted clinician.
We kindly ask that you do not join in the spiteful mob mentality of scapegoating General Practice and its highly committed staff for the faults of society and a broken system based on an outdated model of care, which is the result of decades of deliberate underinvestment and artificially fuelled over-expectation.
Whatever happens, at Ivy Grove, we will always aim to do our best for you
Whatever happens, we, at Ivy Grove Surgery, will always aim to do our best for you to provide you with high quality and family friendly healthcare.
Some of the media interest
PULSE: In full: GP practice’s 16-page letter to patients - April 26 PULSE: GP practice writes 16-page open letter to patients after seeing demand double - April 26 HSJ: Daily Insight: ‘A brand new lane on a full motorway’ - April 30 HSJ: Stretched GP practice writes scathing open letter to patients - April 30 DAILY ADVENT: GP practice writes 16-page open letter to patients after seeing demand double - April 30 ONMEDICA: HSJ: Stretched GP practice writes scathing open letter to patients - April 30 THE TIMES - April 30 REDDIT: Open letter from Ivy Grove surgery - April 30 FACEBOOK: Practice Managers Association - May 1 PULSE: 16 things that are wrong with that 16-page open letter - May 4 BMJ: GPs are at “breaking point” and in need of respite, leaders warn - May 4 PRACTICE INDEX: GPs struggle after patients swamp on-line message system - May 4 AUSDOC: Overworked GPs write open letter to difficult patients - May 4 DOCTORS.NET: GPs hit back after patients swamp on-line message system - May 4 360 MEDICAL CENTRE: An open letter to patients explaining how demand for services has doubled in recent months – An interesting read, penned by a Derbyshire GP practice - May 5 PATIENT SAFETY LEARNING HUB: GPs are at “breaking point” and in need of respite, leaders warn - May 5 YOUTUBE: Are GP online consultations sustainable? - May 5 GP ONLINE: Viewpoint: Patients and GPs are unhappy with access to general practice, what's the solution? - May 6 FACEBOOK: Tonyfelin Medical Centre Caerphilly - May 7 DAILY MAIL: Let us all see our GPs face to face again: Last November The Mail on Sunday first highlighted the fears of patients only allowed phone or video calls with their doctor... by February nothing had changed - nor has it now - May 8 NEWS CHANT: Mail on Sunday launches campaign urging NHS bosses to let us all see our GPs face to face again - May 8 SUNDAY EXPRESS: GPs warned NOT to default to virtual consultations - huge health row to erupt - May 8 AUS DOC: 'Real medicine is nothing like TV': Read the GP open letter to difficult patients - May 11 TELEGRAPH: Special report: How our GP services lapsed into long-term sickness - May 12 DRAYTON MEDICAL PRACTICE: Update May 2021 - May 14 THE LOWDOWN: Is online access to GPs increasing their workload? - May 17 THE LOWDOWN: Is online access to GPs increasing their workload? - May 18 THE SATURDAY PAPER: Medical uncertainty - May 29 MEDLOOP: Primary Care needs evolution, not a revolutionCOUGHS, COLDS, SORE THROATS
Sore throats can last 7 days, coughs and colds can last 3 weeks and most clear with self-care and help from the pharmacy
As the country opens up and people are having more contact with each other, we are being contacted by increasing numbers of patients with coughs, colds and sore throats, generally within a few hours of starting with symptoms and with no attempts at self-care.
These conditions are extremely common, mostly self-limiting and can generally be managed by self-care, and additional help from the pharmacist. The natural history of such conditions is that sore throats can take a week to clear, a cough and cold symptoms can last for 3 weeks. If you are getting no better after these time periods then please do get in touch.
We encourage all patients to follow self-help guidance on these conditions in the first instance. The links below will advise you what to do and include details of worsening symptoms to look out for and when you should contact the GP. They include leaflets written by our doctors for the benefit of all our patients. More leaflets are available.
Also remember that if you develop a new cough, or temperature, then you must book for a PCR covid test, see below for more details.
NHS.UK advice on sore throats NHS.UK advice on coughs NHS.UK advice on colds Minor illness leaflet: Coughs and colds (Dr Axten) Minor illness leaflet: Sore throats (Dr Smith) Get a free PCR test if you have coronavirus symptomsCOVID NEWS UPDATES
As the country opens up, there remains uncertainty about the B.1.617.2 variant of concern (Delta/Indian variant), with some scientists urging more caution in the coming weeks.
As indicated above, in recent weeks we have had to advise more and more people with new upper and lower respiratory tract symptoms, such as cough, runny nose, catarrh and temperature. We therefore think it prudent to give a timely reminder about coronavirus and covid testing which many people appear to have now forgotten.
Outdoors still safer than indoors
The country is still actually in a state of lockdown, with restrictions gradually easing in a stepwise manner. As we mentioned in a previous update, just because you can, doesn't always mean you should, especially given the uncertainty around the new variant at the moment, and the fact that young people have not yet achieved target vaccination rates.
We know we've all been frozen in the garden as the sun sets on our outdoor socialising, but as the weather improves and as the country opens up, outdoor socialising might become more comfortable, and the truth is that outdoors still remains much safer than indoors, given ventilation significantly reduces viral load.
But if you do choose to move your socialising indoors, we advise you to continue to take care with all usual precautions.
Two types of covid test (PCR and lateral flow test)
A lateral flow test (slide test) is only for when you have no symptoms
Temperature, new cough and loss or change to sense of smell or taste remain symptoms that require a covid test. There are two types of covid test: PCR tests, which are sent off to a lab, and rapid covid tests (lateral flow tests), which are slides that you do at home and that give results in 30 minutes. PCR tests are for people with symptoms. Lateral flow tests are for asymptomatic people (people without symptoms).
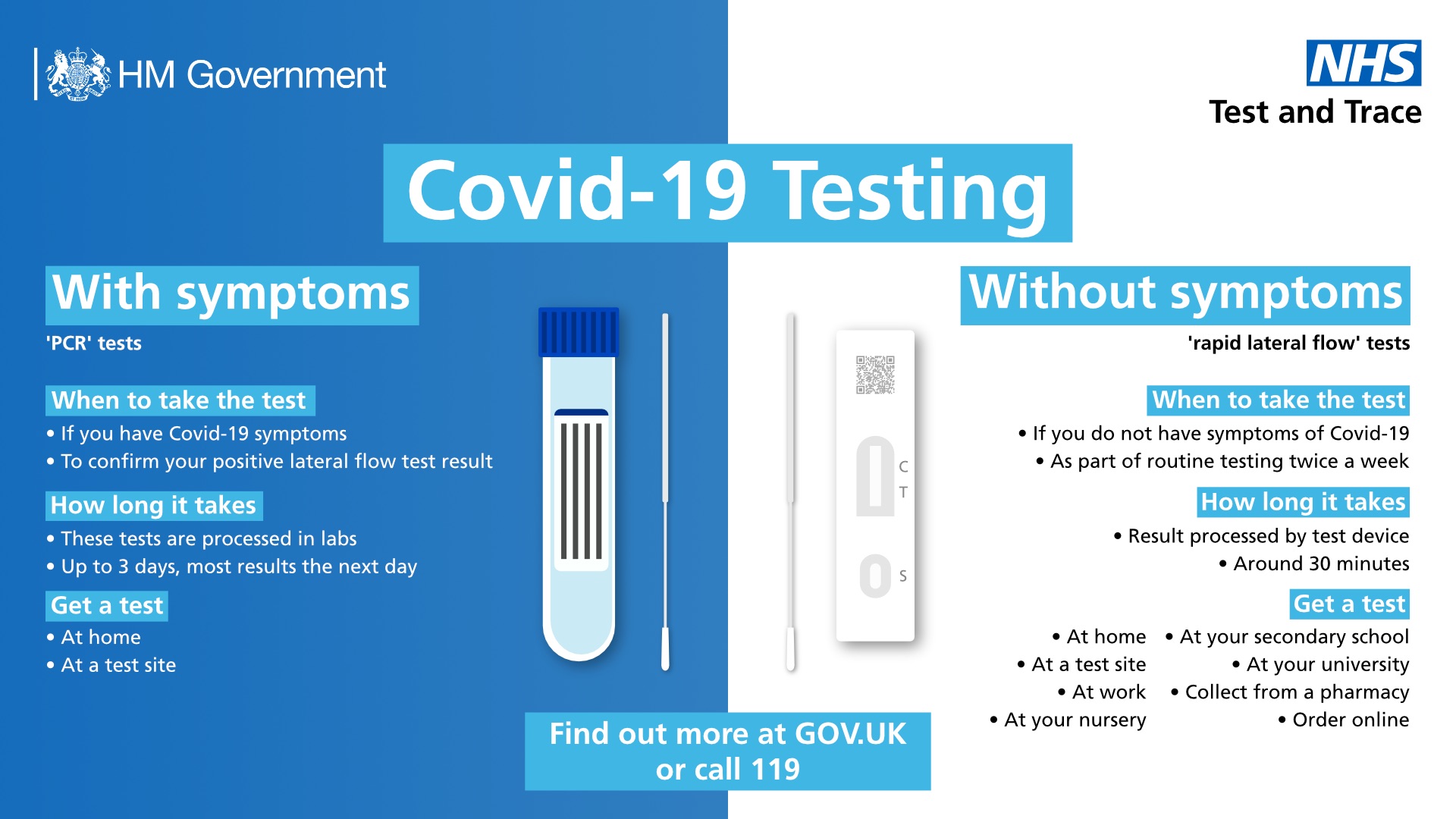
If you have symptoms book for a PCR test
If you have symptoms, book for a PCR covid test - do not use a lateral flow test
Don't use a lateral flow test if you have symptoms. They are not designed for those with symptoms. Book a PCR test and you should get the results fairly quickly, within 24 hours generally. You need to self-isolate until you know the result and the only time you can leave home at all if you have symptoms is when you go for the PCR test.
Get a free PCR test if you have coronavirus symptomsIf you have symptoms book for a PCR test
So important we have repeated this headline twice.
For the sake of yourself, your family, your friends, your work colleagues and your country, please get a PCR test. Testing (and contact tracing), along with vaccination, remains one of the ways to get this country out of the pandemic.
Invalid reasons for not getting a PCR test include:
"My lateral flow test is normal" [incorrect test for this purpose]
"It's my usual infection", "I know it's not covid", "I know my own body" [how do you know?]
"I feel all right" [covid doesn't taken in account if you feel all right; up to 30% of people with covid have no symptoms]
"I just need some antibiotics" [inappropriate treatment for a virus]
If you are one of those thinking this way, please do get a PCR test first. If you still need medical help from us, then please get in touch, but please get a PCR test first. We are still seeing positive results come through for our patients, so covid is still around.
Get a free PCR test if you have coronavirus symptomsSelf-isolate according to the rules
Testing and self-isolating help to protect not only yourself but also others around you
If you are awaiting the result of a test, you and your household must self-isolate until you get the result.
If you are contacted by NHS Test and Trace, you must self-isolate – this is a legal requirement and you might be fined if you don't. Whilst self-isolating, if you don't have covid symptoms, you do not need to get a test. But if you develop covid symptoms, please book a PCR test.
Again, actions to get yourself tested and to follow self-isolation and NHS Test and Trace instructions are to keep not only yourself safe, but others around you and ultimately will help us all.
How to look after yourself at home with covid When to self-isolate and what to do How long to self-isolate If you're told to self-isolate by NHS Test and Trace or the NHS COVID-19 app Get a free PCR test if you have coronavirus symptomsTest regularly according to your educational or workplace setting
Lateral flow testing is to check asymptomatic people. The reason for rolling out these tests widely is to pick up cases of covid in people with no symptoms. 30% of those infected with coronavirus show no symptoms, so it is important to check regularly by following the regime of regular testing as determined by your educational or workplace setting.
You should be supplied with lateral flow tests from your setting, but you can also order them directly. But remember, do not use them if you have symptoms - book a PCR test instead.
Order free rapid lateral flow tests Get a free PCR test if you have coronavirus symptomsThe covid jab doesn't make you invulnerable
As we have mentioned previously, you can still get coronavirus even if you have had the jab (one or both). The aim of the covid jab is to reduce (not eliminate) the risk of serious complications, reduce (not eliminate) hospital admission and reduce (not eliminate) transmission. So, even with the covid jab, there is still a possibility you might get seriously ill, need hospital admission and pass it on to others.
So, please still follow the rules and get tested if you have symptoms, and continue to take the existing precautions of hands, faces and space to reduce the risk further.
Covid vaccination passports - please don't contact us
Please do not contact us about your covid vaccination (covid passport) status - use the NHS App or ring 119
As the country opens up and international travel is reinstated, we kindly ask that you do not contact us with any requests to confirm your covid vaccination status.
Covid vaccination status is available from within the NHS App. For those without smartphones, you can also dial 119 to request a letter.
Please do not contact us as we are already extremely busy with clinical work and your calls about covid passports will risk blocking urgent calls coming in. We have posted some advice on our covid vacc page for your information.
Info on the NHS App Ring 119 Covid vacc pageCovid vaccination in under 40s
We have updated our covid vaccination page to reflect new information about the vaccine in under 40s. In short, for healthy under 40s, it is preferable to have a different covid vaccine from AZ vaccine, however if you have already had the first AZ vaccine without problems, you should still have the second as planned. Please see our covid vaccination page for more information.
Covid vacc pageAccelerated courses
In light of coronavirus variants of concern in circulation, second doses of covid vaccine will be brought forward to 8 weeks rather than the existing 12 weeks, in order to accelerate the program and ensure that people are fully protected earlier. We will post information on our covid vacc page when we hear more.
Covid vacc pageMake sure you get both jabs
Uptake levels of covid vaccination remain high in all groups so far, so well done everybody for attending for your jab and well done to all staff members of the various GP teams who have helped out. But please also make sure you complete your course of two jabs. And please keep yourself safe, even after you have had the jab; immunity takes a few weeks to build up and it has been found that many of those admitted to hospital either had not been jabbed at all, or had caught the infection before immunity had a chance to develop.
Given the accerelated courses mentioned above leading to a peak of vaccinations required to be performed at the same time, it is likely that Ivy Grove will be involved in an afternoon closure so that we can help to jab more patients from the local community - we will notify you in advance of any forthcoming closure. There will be emergency cover provided, but we do advise that on these afternoons, please do look after yourselves, and please bear with us whilst we continue to support the efforts to get the country out of the pandemic.
Historic landmark for Derbyshire as teams administer 1 million Covid-19 vaccinesStop Press - preliminary date for covid vacc clinic set
ZERO TOLERANCE TOWARDS ABUSE
"If I die it will be your fault" (4:11), Institute of General Practice Management, shorter version (2:25)
Sad to report, but abuse against hardworking health care staff is on the rise.
We would like to remind all our patients that abuse towards our staff, verbal, face-to-face, on social media or otherwise will not be tolerated. Life is difficult enough as it is already without having to cope with rude, aggressive and intolerant people.
We appreciate things are difficult for everyone at the moment, and can seem worse when you are poorly or under the weather, however abusive behaviour cannot be excused. Our staff are doing their very best to help everyone under these extremely trying circumstances, and we will always aim to remain polite and helpful.
We do not think it is too much to ask that patients treat our staff courteously at all times. A healthy doctor-patient relationship is the cornerstone of good clinical care, but patients who abuse mutual trust and respect risk being removed from our register.
Abuse of any sort against our staff will not be tolerated
In line with NHS zero tolerance policy, any patient considered to be abusing our staff will be sent a warning letter. A repeated infraction will result in removal from our panel. Any person abusing us on our social media pages will also be banned from our pages and comments will be reported and/or deleted.
Harassment will be reported to the police. Violence or threats of violence of any kind will not be tolerated and will result in the police being notified and immediate removal.
These measures help to support our dedicated staff so that they can continue providing care for you. Thank you for understanding.
MENTAL HEALTH SUPPORT
Many patients are still not aware of the extensive support and help available for those suffering with their mental health, whether it be anxiety, low mood, obsessional disorder, panic, phobia, stress, psychological disorders or other mental health issues.
We have collected these resources over the course of the pandemic to help support our patients through their struggles. We recommend these services to anybody suffering at the current time, so that you can start to get the help that you need. Using these services does not stop you contacting us for additional help if needed - please continue to call in if you need our help.
Start to get the help that you need
Leaflet on counselling and other support numbers including what to do in a crisis Counselling support page All mental health help and support Free 24 hour mental health support line for all age groups information Mental health support line for all age groups 0800 028 0077 Tackling sleep problems Mental health resources for children Mental health resources for teenagers Mental health resources for adults/general Mental health resources for older patients/vulnerable Dementia support services NTW mental health self-help leafletsWhat to do in a mental health crisis
If you feel at imminent risk of self-harm, please seek help urgently. You are not alone. You can ring us, contact NHS111, dial 999, speak to the Samaritans, present yourself to the nearest A&E department, speak to your counsellor, your community psychiatric nurse, the crisis team (if you are under their care) or confide in a trusted friend or family member.
Ring us Ring 111 Ring 999 Ring Samaritans 116 123 Royal Derby Hospital Accident & EmergencyTIMED CALLBACK REQUESTS IN CLINIC
Our morning acute care clinic is a telephone-based clinic where patients will initially be remotely assessed and if clinically necessary, they will be brought into surgery to see us face-to-face. The principle behind this is that it works similarly to the acute care clinic in pre-covid days where patients would need to be ready and available to come to surgery to be seen.
Given that this is not an open-ended clinic, and the fact that we have many other clinical commitments throughout the day (including follow-ups, tasks, visits, paperwork), patients will need to be available for a callback at any point in the duration of the clinic, in case they need a face-to-face assessment during the session. Unfortunately, we cannot promise a specific callback time when the clinic is not running. If this proves unsuitable for you, we kindly ask that you ring back another day when you would be available.
By doing this, we can ensure that we help as many people as possible.
LATEST FEEDBACK
We remain extremely grateful to our kind patients who have supported us through these difficult time, and it is heartwarming to continue receiving your great feedback, some of which is reproduced below.
Thank you for the latest newsletter. The newsletters are very informative and helpful. I feel they keep me in touch. Thank you to everyone at Ivy Grove for all you are doing, especially in the current situation. - RS
Thank you so much for the regular updates which cover every aspect of the current situation. A huge THANK YOU to all staff members for the efficiency of the vaccine clinic which I attended. I regard myself as being very fortunate to be a registered patient with Ivy Grove. Best wishes to you all. - JG
Just wanted to say a big thank you to each & everyone of you for your time and effort in keeping us all who use ivy Grove Surgery safe and as healthy as possible in the times we are in currently. The newsletter you send out is first class so thank you all very much for all the effort you put in keeping us informed. - MC
I would like to commend all the staff at Ivy Grove for the efficient and seamless way they are handing out the covid jabs. Well done to all involved. - LR
I have now had 2 vaccinations at the surgery & would just like to say how efficiently this was carried out. Also to thank everyone involved for everything that is being done to produce a smooth running service at what must be a time of ever increasing workloads. Thank you too for all the up to date relevant information on the website, it is appreciated. - CR
My daughter and I had our covid vaccination today, my daughter has ---- and ----, and taking her anywhere is very difficult, but I have had a few conversations this week with various receptionists and nurses, and I would like to say how helpful everyone was, nothing was too much trouble for them, and they did everything they could to make it as easy as possible, thank you all so much for your help and understanding, it made what could have been a very stressful time a lot easier. - SH
PATIENT INFORMATION LEAFLETS
We draw this long issue to a close with a reminder of the information leaflets which we have written for patients that are available to download on our website. These have been devised by our already busy clinicians in their own time to help and support patients with their conditions. We hope that you find them useful.
NEW Chronic kidney disease (Dr Greer) NEW Diazepam prescribing for fear of flying, dentistry, scans etc (Dr Greer) NEW Folic acid deficiency (Dr Wong) Cardiovascular risk (Dr Wong) Diabetes foot care (Dr Wong) Get the right help for your condition (Dr Wong) How can I tell if my child is poorly? (Dr Wong) Minor illness leaflet: Earache (Dr Francis) Minor illness leaflet: Urinary tract infection (UTI) (Dr Greer) Minor illness leaflet: Thrush (Dr Greer) Minor illness leaflet: Diarrhoea and vomiting (Dr Wordley) Minor illness leaflet: Conjunctivitis (Dr Horton) Minor illness leaflet: Injuries and conditions (Dr Horton) Minor illness leaflet: Bacterial vaginosis (Dr Greer) Palliative care (Dr Smith) Prediabetes (Dr Francis) Sick notes after hospital care (Dr Wong) Steroid injections (Dr Axten) Vitamin D insufficiency (Dr Axten) Vitamin D deficiency (Dr Axten) More leaflets are availablePRINTOUTS OF THIS UPDATE
We realise that amongst those reading, there will be some of you who will have relatives or friends registered with the surgery who do not have internet access or smart devices and who therefore cannot read our monthly updates, where previously they could just walk in and collect a copy of our regular newsletter from the reception desk. To help with this, we have changed settings on this page so that it can be easily printed out on home printers in large-print format, should you wish to do so. You can print directly from your browser (usually CTRL + P or COMMAND + P), or click the button below.
Print this news updateFINALLY...
So, after another super busy month in the land of General Practice, we hope that you will all do your best to look after yourselves during these difficult times, that you will get both doses of the covid jab when it is offered to you, that you will all do your best to keep as safe as possible, and that you all follow current guidelines.
By doing so, hopefully, we can all get out of this sorry state of affairs intact and safely through to the other side.
Kind regards
Ivy Grove Surgery
Written by Dr M. Wong
© Dr Michael Wong 2022