Latest News Update 21.1
March 31, 2023
Dear Patients
This is our latest news update following on from our last one in December. Previous updates issued since the pandemic can be found here.
This is a difficult update to write given the current situation, at a time when GP workload continues to rise without any improvement in GP staffing levels and when attacks on GPs, via news outlets and social media, and even physical assaults, continue to make the news.
On top of this, we have just come out of the Strep A crisis, and come to spring with the threat of a contract being imposed upon us (yet again). Despite all this, we continue to try our best and as part of this, we have various updates to inform you all about.
WEBSITE AND TEAM UPDATES
We continue to update our popular website for the benefit of users.
In response to a review of user journeys and experience of popular pages, sections and documents on our website, we have made improvements to the top navigation (for desktop and tablet) and side navigation (for all devices). These are now more task-based with submenus revised into more logical categories.
So, for instance, one of the commonest task for patients is to find out how to get their repeat medications. To help with this, there is a new option in the top menu for ‘Meds’ and in the lefthand menu, 'Ways to get your meds' is shown in the ‘Popular right now’ heading.
Ways to get your meds (ivy.gs/meds)Ways to get help are other main actions for patients. To help with this the ‘Get help’ heading in the top menu and the ‘Get medical help’ in the lefthand menu have been expanded with options, which do not just include appointments.
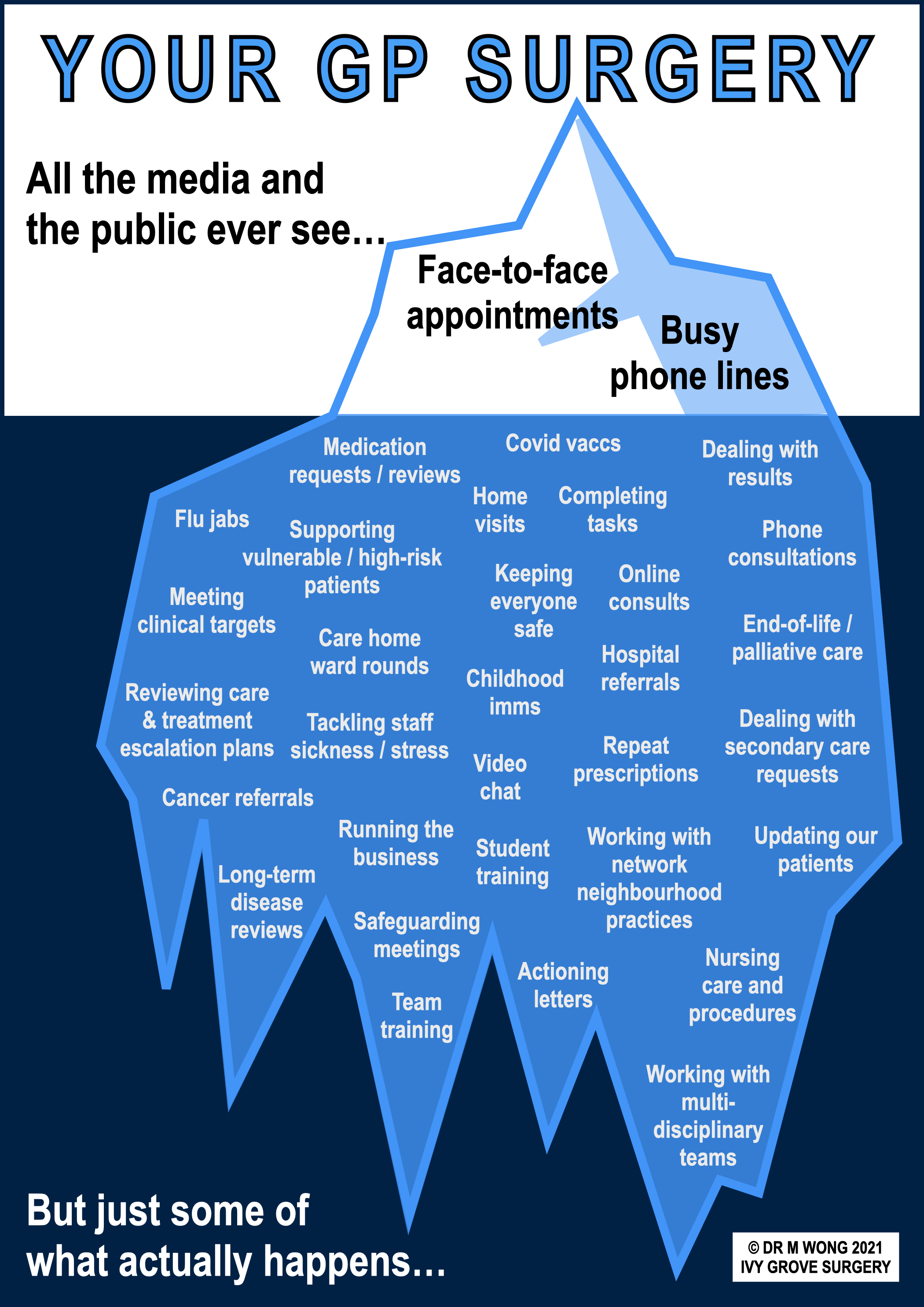
The reason that there are many more options other than just 'appointments' is precisely that reason – there are indeed many more options than just an appointment with the GP. We do need to remind patients that General Practice is evolving – you can now get help from the entire GP team directly , not just the GP. In fact, the GP might not be the most appropriate person to speak to or see first. Please read the official leaflet on changing roles in General Practice.
Roles in General Practice Meet the GP team (ivy.gs/team)Accordingly, our ‘Get help’ options give links to ‘Meet the GP team’ to introduce you all to the different members of the team, to whom you can self-refer directly as well as other NHS workers, again to whom you can self-refer directly.
Our Get help page walks you through the various options for accessing health services and we recommend using it to get the help you need.
Ways to get help (ivy.gs/help) Get the right helpWe continue to promote self-care as a quicker and easier way to recover from minor or self-limiting illness and self-referral as a way for you to access other health workers. All of these options are available to you so that we may maintain a sustainable service. Again options for self-care are in the top and lefthand menus.
Self-refer to others (ivy.gs/selfrefer) Try self-care (ivy.gs/selfcare)We appreciate changes are not always welcome or will often take time to get used to, but we hope that you will bear with us whilst we continue to improve our visitors' experience of our popular website.
The same applies to staffing. Many of you will be used to only ever seeing a GP in your entire lives. Traditionally the GP team was only ever doctors and nurses. But nowadays, given the severe shortage of GPs, we have had to make changes to our complement of health professionals, to continue to maintain our services to patients. Here we introduce some of them.
ADVANCED NURSE PRACTITIONERS (ANPs)
The above mention of the GP team indicates that there are other team members that we need to introduce you to. We have two Advanced Nurse Practitioners (ANPs) working regularly at the practice at the moment.
ANPs are highly qualified nurses able to tackle a range of conditions and minor illnesses, such as joint problems, sore throats, ear infections, conjunctivitis, other eye problems, chest infections, asthma, chronic bronchitis, urine infections, incontinence, thrush, skin problems, rashes, spots, tummy ache, diarrhoea, constipation, indigestion. One of our ANPs also deals with some mental health conditions, dizziness and breast problems.
Although this might represent a change which some patients might not be used to, the introduction of ANPs into the service does bring some benefits to patients. There will be more appointments available and consequently shorter waiting times. The ANP will free up some time for GPs to deal with more complex cases and to maintain a degree of continuity with such patients.
Depending on your condition and their availability, you may be offered an appointment with one of our ANPs. Following assessment, if the ANP feels that you need a GP assessment, you will be advised accordingly.
GP TRAINEES (REGISTRARS)
Dr Neely, our training lead, now writes about our new GP trainees.
Since August 2022, Ivy Grove has been approved as a practice to help train the GPs of the future. We have started with one trainee at a time, but from August 2023 there will be two trainees.
These are fully qualified doctors with several years’ experience in the hospital and some GP experience. We will be helping them to improve further to hopefully pass their gruelling and expensive exams to fully qualify to be a specialist GP.
This brings lots of benefits to the practice. It helps the practice to remain up to date with clinical developments and changes within the local hospitals, it develops the skills of the GPs who supervise the doctors in training as educators and it provides variety to help maintain our enthusiasm for what can be a very challenging job.
It has taken a lot of work and training to be accepted as a practice suitable to host doctors in training and is one indication of high standards of organisation and patient care. Being involved in training is also an advantage for GP recruitment, both by directly training our next colleagues and by enabling us to attract potential recruits due to our training status.
HEALTH AND WELLBEING COACH
Sam, our new health and wellbeing coach and lead coach for the network of local practices, now writes about herself and her role.
INTRO TO LINDSEY
Here, Lindsey, one of our new nurses, introduces herself:
INTRO TO JESS
Here, Jess, our other new nurses, introduces herself:
STAFF TRAINING AND AFTERNOON CLOSING
Like most other responsible workplaces, and especially one where we have lots of different team members performing different roles, we do take the time to regularly train our staff and have development sessions to help improve our performance or services.
During this time, urgent cover is provided by the out of hours service by ringing the normal surgery number. We post details of our staff training dates throughout the entire year on our website, on the staff page and in advance on the home page.
Some of these training sessions are mandated by the network of nine practices in the Amber Valley area (called Alfreton Ripley Crich Heanor Primary Care Network, or ARCH PCN for short), and accordingly, during these times, all nine practices in the local area are closed in the afternoon.
Despite this closure affecting all local practices, and despite the fact that urgent cover is still provided to those in clinical need, we are sad to report that several disgruntled patients have felt the need to post negative comments on our Google business page unhappy that they have found us closed on a Wednesday afternoon.
We hope that those leaving such reviews will appreciate that such closure, although inconvenient, is a small price to pay and is in the interests of all patients so that we ensure all our staff are well trained in order that they may provide safe, effective and caring service.
Staff training dates Get help when we're closedPLEASE LABEL YOUR SPECIMEN BOTTLES
Just a brief reminder to all patients submitting specimens to us, to please label your urine and stool bottles, sputum pots and swabs with your name, date of birth, date and type of sample. Failure to do so will result in the lab not testing the sample and inconvenience from having to repeat the test.
URINE SAMPLES
In order to provide important clinical background and to make the correct clincial decision, we now require a form completing for urine samples that have been dropped off at the reception desk. We have had to introduce this move as we have had many urine samples handed in over the desk, which have not been requested by us, and for which we have no information on which to base any decisions on treatment (if any).
The form, which is available below, will ask some questions regarding the condition of the patient and if they are suffering with any symptoms suggestive of an infection. Please do not be offended when asked to complete a form with your specimen, but failure to do so may result in your urine sample being declined. You will be handed a form to complete at the reception desk.
Please note that the above process does not apply if you are bringing back a urine sample that we have specifically requested and which is already accompanied by an official laboratory request form.
Urine sample formHIGHLY QUALIFIED TRADESPERSON REQUIRED
Exciting job opportunity – apply now
I am looking for an annual contract renewed each year in perpetuity with a highly qualified tradesperson who is a plumber, electrician, painter, decorator, plasterer, gardener and odd job person to provide services for me please. It is essential that you have all the above skills and qualifications as I may not always know what I will be needing from you when I contact you.
As part of this contract, I will be able to call you out as many times as I like, subject to your phone line not being constantly engaged, as given the terms of this contract, I know you may well be quite popular. At no time during the contract will I be paying any call-out fee.
You will provide me with any and all of the services specified, and will not be able to charge me any fees at any time, nor any additional fees for providing me with any other additional services of the above type that I might wish for or that you might wish to provide me with, outside of the specified contractual requirements.
You will need to be available to me at any point between 8.00am and 6.30pm Monday to Friday. Outside of these times, I am willing to pay you the sum of £4.73 per year, to have access to an emergency service to sort me out, until you, as my contracted tradesperson, will again become available. Again, I must stress, I will not be paying any fees or any call-out fees at any time whenever you tend to my needs.
Tradespersons who have not done the required minimum ten years of training need not apply. Furthermore, as part of this contract, you will need to undergo a rigorous annual assessment by peers, be inspected annually by a series of overzealous regulators, the services for which you will need to pay yourself. This scrutiny is required as otherwise I will assume that you will be working to completely outdated procedures, are totally unethical and will always be wanting to cheat me, or worse, bump me off.
Finally, I demand that you will not make any mistakes in your work whatsoever, otherwise I will be forced to complain vigorously to anything up to 20 different organisations, who will investigate you and to which you will be required to respond in immense detail within strict timeframes, the consequences of such investigation which may include the loss of your livelihood.
This is a wonderful opportunity for any professionally qualified tradesperson and I am prepared to offer this contract to you for an extremely generous £99.70* per year.
Sounds incredible doesn't it? How many of you will find a tradesperson like that willing to sign up? Most would laugh down the phone at you.
Well, that is exactly what your GP gets to provide you a service for a year, and what is expected of them. Now can you see why there are no applicants for such a position, and why so many GPs are leaving the NHS? And can you see why, when many others are demanding the same level of service from fewer and fewer GPs, why you can’t ever get an appointment?
GP CONTRACT ARTICLE
If you wish to share this article, or need to come back to it at a later date, use the shortcut ivy.gs/gp-contract
IMPOSED GP CONTRACT
The above parody advert for a contract with a highly qualified tradesperson was adapted from social media, but it is uncannily accurate, and highlights the GP contract, which some of you may have heard about on the news recently.
What now follows is a detailed commentary on the GP contract. We make no apologies for bringing this to the attention of our patients as it has the potential to adversely affect the care you may receive from the surgery. As we have done for many years already, we will continue to engage with our patients around the wider aspects of General Practice, as unfortunately external factors, such as politics and the media, have a very unhealthy influence (no pun intended) upon what should be privileged interactions and a valued and long-term relationship between doctor and patient.
SOME HISTORY
A little history lesson follows as an important prelude to some discussion about the current situation. One of the main things we learn from history is that we don’t learn from history, because humans tend to have short memories, so we feel it is quite important to recount this tale of how General Practice has got to the sorry state it is now in.
In 1997, New Labour were voted in. In response to declining investment and recruitment and retention problems in General Practice, a new GP contract was negotiated in 2004.
Back to the contract now, and unfortunately, but relevant to the current situation, embedded in this contract was a clause that enabled the government to impose changes to the contract with 12 weeks 'consultation'. Concerned by the presence of this clause, GPs were reassured by both the government and GP leaders at the time that this clause would only ever be enacted in times of national emergency, such as war, acts of terrorism and environmental disasters.
Back to history now, in 2008, only four years into the new GP contract, as part of Gordon Brown wishing to secure his legacy for the NHS, despite his very short tenure, Labour exploited the imposition clause for the first time and imposed the contract forcing GPs to work 12 hour days to regain funding deliberately removed from the contract. This was called ‘extended hours’. At the time, there was no national emergency cited as a cause for this contract imposition.
In 2010, the Conservatives were voted in. In 2013, they exploited the imposition clause too and imposed a contract resulting in funding cuts and increased workload by chasing spurious targets [indeed regarding this contract imposition, the author wrote to the Health Minister at the time, one Jeremy Hunt, now Chancellor, but without success]. Again, at the time, there was no national emergency cited as a cause for this contract imposition.
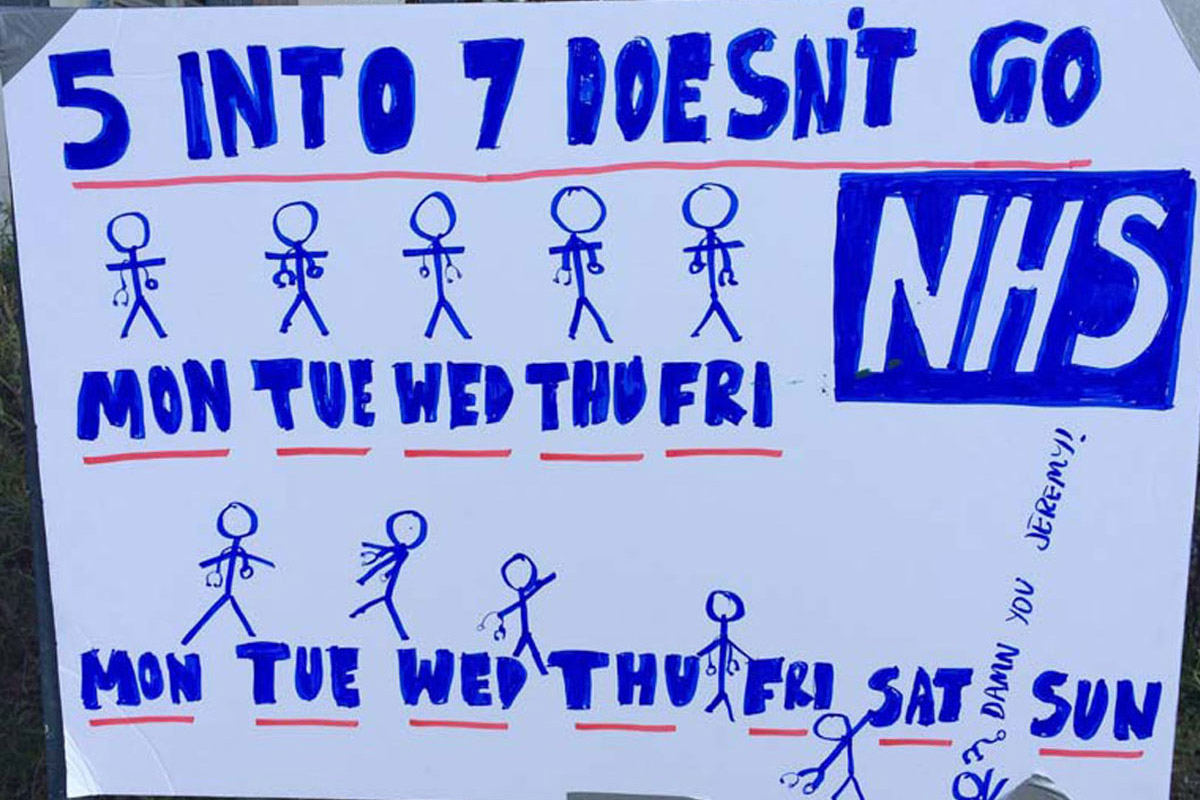
In 2015, the Conservatives won the general election and, as part of David Cameron wishing to secure his own legacy for the NHS, he promised a 'world-leading' 7 day NHS - that is, 8am till 8pm opening 7 days a week – this was known as ‘extended access’. This was met with huge resistance from the junior doctors (expressed from the point of view of lack of staff to cover and concerns over patient safety) but unfortunately the end result of this debacle was that Jeremy Hunt imposed a contract upon them. Junior doctors have remembered this ever since and are now getting their own back.
In 2018, extended access started in GP land and was deliberately funded at twice the cost of daytime General Practice, immediately skewing clinical priorities and staffing cover for political purposes [again, imagine if the funding had been directly provided to General Practice to cover daytime opening hours].
In 2019, the GP contract changes forced practices to join together to form networks of GP surgeries, called Primary Care Networks (PCNs), with removal of funding from individual GP surgeries, moving it to these networks on the proviso that the networks would reclaim the funding through hiring of a specific set of new staff as determined by NHS England [as previously mentioned, no GPs and nurses at all could be hired with this funding and if the specific staff could not be hired, networks would lose the funding; crazy when we are crying out for GPs and nurses and equally crazy to lose the funding].
In 2022, the Conservatives exploited the imposition clause again, so for the third time so far, and they imposed the GP contract forcing GPs to deliver services 8am to 8pm weekdays and 9am to 5pm on Saturdays, what is known as ‘enhanced access’. Again, there was no national emergency cited as a cause for this contract imposition.
We now come to 2023, and yet again, the Conservatives have exploited the imposition clause, for two successive years, and they have imposed a contract forcing GPs to skew clinical priorities by focussing almost exclusively on access. Yes, you've guessed it, no national emergency has been cited as a cause for this contract imposition.
So what we have learnt from our short history lesson is that in just under two decades, the government, of various persuasions, has exploited a specific clause in the GP contract no less than four times, a clause that was only meant to be used at a time of national emergency, and inappropriately used it to push their own political agendas and their own selfish will upon GPs.
Indeed, you will notice that all four contract impositions have been about increasing GPs' already long working hours and pushing access above all else, whilst simultaneously failing to recognise and act upon the dire shortage of GPs, other than trying to outdo each other on the thousands of extra GPs they can promise.
It is also interesting to note that, in the only genuine national emergency of recent times, the covid-19 pandemic, no contract changes were imposed upon GPs. In fact, the contract was relaxed, quite appropriately, in order to support GPs in continuing to provide services to the population whilst also supporting them to deliver the vast majority of the vaccination programme, thereby helping to take the country out of the pandemic.
As the country came out of the pandemic, just as quickly as the grateful clapping from the public turned to violence and abuse, we have now had two contract impositions in quick succession. This indicates quite clearly the intentions of the government going forward.
So all of this brings us to the current imposed GP contract. But before we do so, we need to introduce some further background information.
SOME CONTEXT
We won’t repeat everything that we explained in great detail in our GP workforce article, but it is important to provide some background context to the crisis in General Practice, so that the significance of the harm from the imposed contract may be understood. These are genuine figures based on official data.
GP workforce article (ivy.gs/gp-crisis)1,600 GP surgeries, representing a fifth of all practices, have closed since 2013 (GP Online)
At least 1.5 million patients have lost their own GP since 2013, and had to register elsewhere, sometimes at a GP surgery many miles away (Pulse)
Instead of the many thousands of extra GPs promised by politicians as above, 1,622 full-time equivalent GPs have actually left the service since 2015, around 7% of all GPs (NHS Digital)
62 million patients are now registered with GPs, an increase of 7% from 58 million since 2016 (House of Commons Library research)
There are now 2,273 patients per fully qualified GP, up from 1,981 patients per GP in 2016 (House of Commons Library research)
The above equates to just 44 GPs per 100,000 patients, one of the lowest amongst comparable countries (BMA)
26.8 million appointments (not including covid vaccinations) were provided by GP surgeries in December 2022, compared with 25.2 million the same time last year, in December 2021 (NHS Digital)
30 million appointments were provided by GP surgeries in January 2023, an increase in 11% compared to the same time three years ago, pre-pandemic, in January 2020 (NHS Digital)
68.3% of appointments were provided face-to-face in December 2022, compared with 61% the same time last year, in December 2021 (NHS Digital)
48.1% of appointments were provided on the same day in December 2022, compared with 45.8% the same time last year, in December 2021 (NHS Digital)
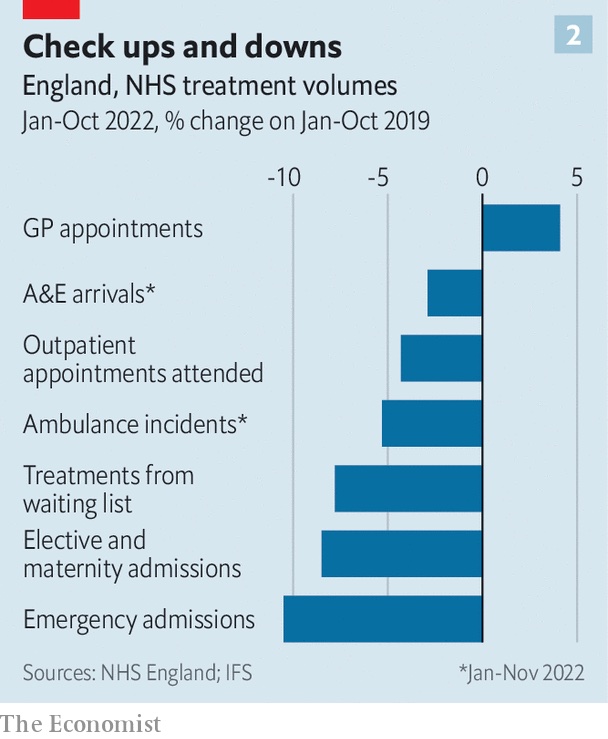
General Practice is the ONLY sector in the NHS to see an increase in productivity when compared to pre-pandemic levels (NHS England) - see graph above/right
The gist of all of the above, supported by official figures, and available to anybody willing to do a little research, is that there are fewer GPs, and GPs and their teams are doing more. But you may already guess how things are, from your own personal experience, even without having to do any research.
Yet the public perception, the media coverage and the political soundbites give the impression that GPs are lazy, earning too much, not doing much at all, not seeing patients face-to-face, their staff are not answering the phones and they are closed to patients. And not only that, when you do get to see them, they don’t know anything, they misdiagnose you, and all they ever do is dish out antibiotics, give you a sick note or refer you to the shiny hospital to see a proper doctor!
It’s against this backdrop of public perception and political interference that the new GP contract has now been brought in and imposed upon GPs.
THE CONTENT
Ironically the letter from NHS England regarding the imposed GP contract starts with more platitude than gratitude, with empty thanks for all the hard work from GPs and their teams, followed by detail that then indicates that they want us to work even harder and provide even more with no additional funding.
We’re not going to give a blow by blow account of what exactly is in the imposed GP contract, it is publicly available after all, but the main points, along with our brief comments are as follows:
Patients to be offered an assessment of need, or signposted to an appropriate service, at first contact with the practice and not be told to contact the practice at a later time, and networks of practices to work together to achieve the above – this focus on access in the imposed contract is one of the biggest sticking points in the contract and will be discussed in more detail later.
Records access will be provided from October 2023 – we will post fully on this in due course, but a warning to patients that having access to your records is not without the risk of sharing it inadvertently with a third party – global records access without thorough checks from your GP for harmful material, or a consideration of the dangers of sharing could put the vulnerable, those being coerced, or those with poor mental health at risk.
Cloud-based telephony and specific requirements and providers will be mandated – GPs must upgrade their telephone systems from a specific list of providers and with specific functions enabled, all at their own expense. Talk about control.
With not a hint of irony, further ‘quality improvement’ changes to the contract involve ‘optimising demand and capacity in General Practice’ along with a ‘focus on workforce wellbeing’ – we would argue that focussing on providing more access is entirely at odds with ensuring the health and wellbeing of our already pressured staff. As we understand it, there are no real resources available for improving staff wellbeing, with only lip service being paid.
Linked to this contract is the legal requirement for GPs to declare their earnings. This is under the stated premise of ‘pay transparency’ in the NHS. However this ‘pay transparency’ does not apply to any other worker in the NHS. Not consultants, not private contractors, not dentists. Only GPs. GPs are actually self-employed independent contractors to the NHS, not public servants, so for us to be singled out like this, well, it’s really in keeping with everything else that is happening around us. At the end of the day, how much your GP earns has absolutely nothing, nothing at all to do with patient care.
There will be changes to the staff that can be employed by practice networks – reassuringly, practice networks can now employ Advanced Clinical Practitioners, which are a form of nurse, but at a level of only three per 100,000 patients. This equates to around one-third of a person per average practice – neither use nor ornament to any practice we argue – but if we are getting a third of a person, please can we have the bit that talks and can move its arms, thanks.
COMMENTARY
GPs have not asked for much. All we have asked for is a reduction in the micromanagement, the bureaucracy, the targets and the reporting requirements that plague our everyday lives. Working to 70-odd clinical targets does take its toll and skew our priorities towards patients, who are actually people, not numbers. But when we are actually paid by numbers, there will always be a conflict.
All we have asked for is to have the government provide some support for the cost of living. With energy and consumable costs rising, with minimum wage increases to pay for, costs are going up for all GP partners as managers of small to medium businesses. Rising costs and expenses would put GP surgeries at risk of being unable to hire staff, being unable to maintain services and this would ultimately risk closure. You might argue, well, why should GPs be singled out for help from the government?
You would be absolutely right in your argument, except for the fact that the government has already chosen to support hospitals, trusts and other large organisations, who have much deeper pockets than any GP surgery, with a staggering £1.5 billion to help with inflation costs, yet it has specifically declined to provide similar help to GP surgeries.
HSJ: Exclusive: Trusts and systems to be given £1.5bn to cover inflation costsAll we have asked for is for the money to follow the work, that is, for the funding that is allocated to hiring additional staff be moved back to GP surgeries or networks of GP surgeries and for those GP surgeries to then be able to hire their own staff according to need [as mentioned before, if the additional staff are not hired, networks of GP surgeries lose access to the funding]. Even now, the government has steadfastly refused to allow any of the funding to be used for the hiring of GPs. This is absolutely crazy when we are dying for more GPs and you must question the motives of the government for this deliberate act of omission.
Pulse: Underspent ARRS millions ‘set to be returned to Treasury’All we have asked for is for the government to listen to a profession in crisis, one that is struggling to cope, one that is providing more and more with fewer and fewer. You will remember from above that General Practice is the only sector that has seen consistent increase in productivity whilst actively still losing staff.
But what did we get instead? What we got was a contract that has pandered to public misconception about GPs not providing enough, a contract that is wildly ramping up unrealistic expectations for GPs to provide even more, a contract that aims at micromanaging GPs in the extreme, a contract that aims to fuel increased hatred and vitriol against GPs.
ACCESS AHEAD OF PATIENT SAFETY
Why are GPs so up in arms about this particular imposed contract? It all boils down to a reduced ability to maintain safe practice.
All the access target will do is put GPs and their teams under more pressure to perform, to offer appointments when there are none left, to offer advice when it might be inappropriate, to rush to assess when there is no time.
We as GPs would love to provide more access. But to do this, we actually need more GPs. We need more staff. We need more investment in our practices. What we don’t need are more targets. More requirements. More pressure. We need colleagues and we need the funding to pay for those colleagues. It could not be clearer than that.
The Daily Wail has already jumped on the bandwagon of the new GP contract to use as a stick to beat us with and to force GPs to offer patients appointments at first point of contact. Cloud-based telephony as mandated by government has been hailed as the answer to all the problems. Don't worry as we obviously have plenty of cloud-based receptionists to answer those cloud-based calls.
The questions to ask the average sensible reader would be, when fewer and fewer GPs are providing more and more appointments already, where do people think these appointments will magically come from? Where are the magical receptionists to answer the magical multiple phonelines in the sky to book into these magical appointments? Where are the magical GPs who would see all these patients?
If GPs could break the laws of physics to provide even more with even less, well, we wouldn’t be GPs. We’d all be Nobel Prize winners. Or magicians.
Ultimately the reason why this access target is so concerning to GPs is for the reason of patient safety. If we squeeze even more into the day, because we are forced to, we cannot provide safe care to patients. We know some of our colleagues are each dealing with 50, 60 or 100 contacts in a day, we therefore ask how on earth can anyone be sure that they are providing safe care?
Let’s do some maths. There are 10½ hours or 630 minutes in a GP’s working day, from 8.00am to 6.30pm. At 60 contacts a day, this is 10½ minutes for each patient, back to back, all day. Any time for having a pee, eating, having a drink, dealing with letters or results, dictating a letter, discussing with a colleague or anything not directly in front of or on the telephone to a patient will eat into this time, meaning even less time for each patient. At 100 contacts a day, that’s 6½ minutes for each patient. Again, even less time for each patient, if you factor in additional tasks. Going at that rate is not safe for any GP, not matter how experienced and efficient they are. And certainly not safe for patients at all.
The end result of having less time is that we will rush through clinical assessments, we will miss things, we will make mistakes. We will rush through dealing with paperwork, results, admin, we will miss things, we will make mistakes. Mistakes have the potential to cause harm to patients. Patients don’t tend to like that. Indeed, in recent years, there has been far less tolerance and understanding that GPs are actually humans too, and like all other humans, we make mistakes, especially when under intense pressure.
This point about maintaining safe working at all times needs to be stressed, because, as you will notice, when it comes to pushing access, patient safety is never mentioned by the media nor by the politicians. The reality is that patient safety underpins every decision we make in General Practice. Indeed it is the single most important thing in any provision of healthcare. Patient safety is more important than giving the public what they think they want. Patient safety is certainly vastly more important than the personal whims of any politician after a few votes.
And even if we do try and manage these increased patient numbers, there's going to be consequences upon safety. Let’s be honest, the only way any GP will ever try to manage this, is not to rush through each patient every five minutes. It will actually be to give each patient the necessary time and that means working longer and longer hours to fit all they need to do into the day. The end result will be that overworked GPs will run the risk of stress, burnout, sickness or worse still. A stressed or burnt out GP is no good to any patient. A sick GP offers even less.
If even more GPs leave the service, and there is no suggestion that the rate of departure will slow, given conditions continue to deterioriate, this means even fewer GPs to manage increasing workloads, further jeopardising patient safety. It will put GP surgeries at even greater risk of becoming unviable businesses. This doesn't help patients, and certainly doesn't help GPs and their hardworking teams.
Have we made all this up? No, we’ve not. Please check the following analysis, only just published on March 22, 2023:
HEALTH FOUNDATION: Stressed and overworked - What the Commonwealth Fund’s 2022 International Health Policy Survey of Primary Care Physicians in 10 Countries means for the UKStressed and overworked
What the Commonwealth Fund’s 2022 International Health Policy Survey of Primary Care Physicians in 10 Countries means for the UK
Here are some notable quotes from the report:
GPs in the UK are under extreme strain and public satisfaction with general practice has plummeted
The experience of GPs in the UK should ring alarm bells for government. 71% say their job is ‘extremely’ or ‘very stressful’ – the highest of the 10 countries surveyed
Things have been getting worse for UK GPs. Stress is up 11 percentage points since 2019 and job satisfaction has fallen
The pandemic has taken a heavy toll, with UK GPs experiencing higher levels of emotional distress and bigger rises in workload than GPs in nearly all other countries. UK GPs are among the most likely to plan to stop seeing patients regularly in the next 1 to 3 years
Decisive policy action is needed to improve the working lives of GPs in the UK – including to boost GP capacity and reduce workload. Policymakers considering options for primary care reform should recognise the strengths of general practice in the UK and work with the profession rather than against it – not least because retaining GPs and other primary care staff is essential for the long-term sustainability of services
At this point, it would be worth sharing a report from Sky News where Niall Paterson spends the day on the frontline at a GP practice in Cheshire, meeting staff and patients to uncover the pressures the practice face during a time when the healthcare system is on its knees.
NEXT STEPS
GPs and their leaders are now considering their next steps against this imposed contract. The line in the sand is clear. Patient safety is at risk. If we do not act in some way to get the staff or the funding that we need, then harm to patients will steadily increase. Indeed, patients are already being harmed by not being able to access the services they need because those services are constantly swamped by demand.
We will see what happens, but 'something must be done, doctor', before it’s too late.
Despite all that negativity, please know that we are all still striving to do our very best for you. We know that sometimes our best won’t be good enough and you won’t be happy. For that we wholeheartedly apologise. But we are still trying hard. We are trying hard to recruit more staff. We are trying novel ways to meet demand. We are looking at changes to improve the phone system. But we know it is difficult for everyone on both sides. It therefore warms our hearts to know that some of you still really appreciate what we are trying to do for you.
POSITIVE FEEDBACK RECEIVED
We continue to welcome positive feedback on our services, which we share with the whole team. It is heartening to know that the number of positive messages is still many times higher than the number of negative ones. The following is a selection received recently, some of which the authors themselves may recognise:
Thank you so hard for trying to make me more comfortable – AT
I just wanted to say, every single member of staff I have ever come into contact with at Ivy Grove has been polite, caring, friendly and given excellent customer service. Nothing is ever too much trouble - thank you so much to the reception team! I also wanted to thank Dr Olaoke who I recently had an appointment with and was really caring and informative. Ivy Grove is an excellent GP practice and I cannot speak highly enough. Thank you! I feel lucky to be a patient here and have this as my local doctors surgery. I know the difficulties you are facing right now but each and every one of you is incredible. Have a lovely Christmas. – HA
Thank you for all your help this past year – AW and GW
Thank you for all your help – SI
Thank you for all your help, kindness and care over the past year, take care, stay safe, I really appreciate all of you – DP
Thank you for being so caring and understanding – CB and AB
Thank you for your kindness Emma (receptionist) – PC
Dr Zaklama is the best doctor I have ever had at Ivy Grove, absolutely superb and a 10 out of 10 – KM
Just to say how fabulous Dr Marval was, and I really appreciated the text message this morning, she was very thoughtful - SM
Stellar job Ivy Grove employees are, I can't fault the service I have received from all the people at Ivy Grove, from the receptionist to the doctors, everyone has gone out their way to help me. Now that I'm struggling with awful health, I must have cost much more than is allocated, yet Dr Greer has gone out of her way to help me with this downturn with my health, which can be frightening at my age. So come on everyone be thankful that we have such dedicated staff and cease to denigrate them, you will be lost without them - SH
EMERGENCY ALERTS AND DOMESTIC ABUSE
Emergency Alerts is a UK government service that will warn you if there is a danger to life nearby.
On Sunday, April 23, 2023, all 4G and 5G compatible phones will receive a test text message from the UK government's emergency alert system. Information on this system and the planned test can be found at the link at the bottom of this section.
A 10 second alarm with vibration will sound even on phones which have been silenced.
Victims of domestic abuse who have a concealed phone hidden from their abuser should consider whether to opt out from the emergency alerts on their concealed phone. Please note that simply silencing your phone will not stop the transmission or noise of these alerts. If your phone is switched off or in airplane mode, it will not receive an alert.
Instructions on opting out of emergency alerts follows, or check the video link below.
To opt out on iPhone
- Search your settings for ‘emergency alerts’ and turn off ‘Extreme Alerts’ and ‘Severe alerts’
- If this does not work, contact your device manufacturer
To opt out on Android
- Search your settings for ‘emergency alerts’ and turn off ‘Extreme Alerts’ and ‘Severe alerts’
- If this does not work, contact your device manufacturer
To opt out on Huawei
- (on devices running EMUI 11 or older)
- Search your settings for ‘emergency alerts’ and please turn off 'Extreme threats', 'Severe threats' and 'Show amber alerts'
- If this does not work, contact your device manufacturer
GOV: Emergency Alerts GOV: How emergency alerts work IGS: Domestic abuse poster and resources Refuge: Managing Emergency Alerts on your phone Ring Domestic Abuse Helpline 08000 198 668 Email Domestic Abuse Helpline DERBYSHIRE.GOV: Domestic abuse GOV: Domestic abuse Social care page
FINALLY...
Phew! Having been through all that, please let’s try and end on a positive note. We have some semi-regular nurse practitioners helping with workload. We will be having regular GP trainees. We have a couple of new nurses who are also in active training to develop additional skills. We have a new practice manager who is making great strides with new developments and helping to get the practice back on track. Overall we have a great GP team which is motivated to improve. We have some lovely patients who really do appreciate what we do for them.
Going forward, we kindly ask that all of you carry on bearing with us whilst we continue to try and do our best for you. Till next time.
Kind regards
Ivy Grove Surgery
Written by Dr M. Wong
© Dr Michael Wong 2022